19+ Barriers of Therapeutic Communication Examples
Barriers of therapeutic communication are obstacles that hinder effective interaction between healthcare providers and patients. These barriers can significantly impact the quality of care and patient outcomes. This guide explores the definition, examples, origins, history, and methods for overcoming these barriers, along with practical tips. It includes communication examples that illustrate common hurdles in therapeutic settings, such as language differences, emotional distress, or misinterpretations, and provides strategies to enhance understanding and empathy in patient care.
What are the Barriers of Therapeutic Communication?

Barriers of therapeutic communication in healthcare include factors that impede effective interaction between healthcare providers and patients. These barriers can be emotional, such as anxiety or discomfort; cultural, like language differences or varying health beliefs; and environmental, including noise or lack of privacy. Misunderstandings and lack of clarity in communication also contribute to these barriers. Recognizing and addressing these obstacles is crucial for effective patient care and building a therapeutic relationship.
- Language Barriers: One of the most common barriers to therapeutic communication is a language barrier. When a patient and healthcare provider do not share a common language, it becomes challenging to convey information accurately. This can lead to misunderstandings, misdiagnoses, and a lack of trust. Translators or interpreters can be valuable in overcoming this barrier.
- Lack of Empathy: Empathy is a key component of therapeutic communication. When healthcare providers fail to empathize with their patients, it can create a barrier to effective communication. Patients may feel that their concerns are not being heard or understood, leading to frustration and mistrust.
- Physical Barriers: Physical barriers, such as a noisy or chaotic environment, can disrupt therapeutic communication. Patients may find it difficult to concentrate or express themselves in such settings. Ensuring a quiet and private space for communication can help overcome this barrier.
- Psychological Barriers: Psychological barriers, such as anxiety or fear, can hinder a patient’s ability to communicate effectively. Patients who are anxious or fearful may struggle to articulate their symptoms or concerns. Healthcare providers should create a supportive and reassuring environment to address this barrier.
- Cultural Differences: Cultural differences can lead to misunderstandings and misinterpretations in therapeutic communication. Patients from diverse cultural backgrounds may have different communication styles, beliefs, and expectations. Healthcare providers should be culturally sensitive and aware to bridge this gap.
20 Barriers of Therapeutic Communication Examples
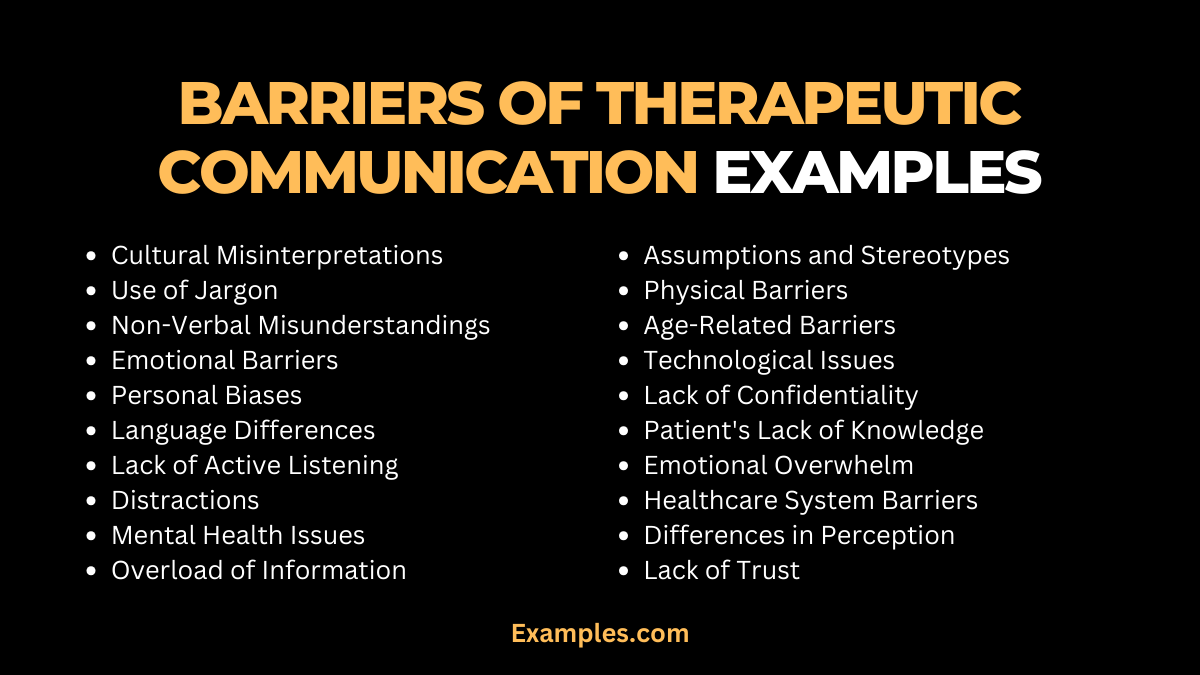
Therapeutic communication is essential in healthcare and counseling, but various barriers can hinder its effectiveness. Recognizing and overcoming these obstacles is crucial for successful interactions between healthcare professionals and patients. This guide delves into 20 common barriers, providing real-life examples and explanations. From cultural misunderstandings to emotional defenses, each example highlights the challenge and suggests ways to navigate these communication hurdles.
- Cultural Misinterpretations: When a therapist misunderstands a patient’s cultural reference, leading to confusion.
- Example: A therapist misinterprets a patient’s cultural expression of distress, responding inappropriately.
- Use of Jargon: Overly technical language creates a disconnect.
- Example: A nurse uses medical terms that a patient doesn’t understand, causing confusion and anxiety.
- Non-Verbal Misunderstandings: Body language that conveys a different message than intended.
- Example: A counselor’s crossed arms may be interpreted as disinterest, even if they are simply cold.
- Emotional Barriers: Patient’s emotional state interfering with communication.
- Example: A patient’s anxiety prevents them from expressing their concerns clearly.
- Personal Biases: Therapist’s preconceived notions affecting interpretation.
- Example: A therapist’s bias regarding a patient’s background influencing their response.
- Language Differences: Language barriers complicating understanding.
- Example: A patient speaking limited English struggles to convey their symptoms.
- Lack of Active Listening: Inadequate listening leading to misunderstandings.
- Example: A doctor misses crucial information due to multitasking during a patient’s explanation.
- Distractions: External factors disrupting the communication flow.
- Example: Constant interruptions during a therapy session hinder effective communication.
- Mental Health Issues: Patient’s mental condition impacting communication.
- Example: A patient with depression struggles to articulate their feelings.
- Overload of Information: Providing too much information at once.
- Example: A pharmacist gives complex medication instructions too quickly for a patient to comprehend.
- Assumptions and Stereotypes: Making assumptions based on stereotypes.
- Example: Assuming a patient’s compliance with treatment without confirming their understanding.
- Physical Barriers: Environmental factors that limit interaction.
- Example: Poor room layout in a counseling session creating a sense of distance.
- Age-Related Barriers: Differences in age affecting communication.
- Example: An older patient finds it hard to relate to a much younger therapist.
- Technological Issues: Technology failures impeding communication.
- Example: A telehealth session disrupted by technical glitches.
- Lack of Confidentiality: Concerns about privacy affecting openness.
- Example: A patient hesitates to share sensitive information in a semi-private hospital room.
- Patient’s Lack of Knowledge: Inadequate understanding of medical conditions.
- Example: Miscommunication due to a patient’s lack of awareness about their illness.
- Emotional Overwhelm: Emotional responses overpowering rational communication.
- Example: A patient becomes tearful and unable to discuss their diagnosis.
- Healthcare System Barriers: Systemic issues causing communication gaps.
- Example: A lack of time for thorough patient consultations due to scheduling pressures.
- Differences in Perception: Varied interpretations of the same situation.
- Example: A patient perceives a diagnosis differently from the doctor, leading to miscommunication.
- Lack of Trust: Distrust in the healthcare provider affecting communication.
- Example: A patient withholds information due to a lack of trust in their doctor.
What are the Techniques to Overcome Barriers of Therapeutic Communication?
Overcoming barriers to therapeutic communication is essential for providing patient-centered care. One effective technique is to use plain language, avoiding medical jargon and complex terminology. This ensures that patients can understand and actively participate in their care. Active listening is another valuable technique, where healthcare providers genuinely listen to patients’ concerns and feelings.
- Active Listening: Active listening involves giving the patient full attention, maintaining eye contact, and providing verbal and nonverbal cues to show that you are engaged and interested. This technique helps patients feel heard and valued.
- Use of Plain Language: Healthcare providers should avoid medical jargon and use plain, understandable language when communicating with patients. Simplifying complex medical information can enhance comprehension and reduce communication barriers.
- Ask Open-Ended Questions: Encouraging patients to share their thoughts and feelings by asking open-ended questions can promote meaningful conversations. These questions invite patients to provide more than a simple “yes” or “no” response.
- Empathetic Responses: Demonstrating empathy by acknowledging patients’ emotions and concerns can help build trust and rapport. Simple gestures like a comforting touch or a reassuring nod can convey empathy effectively.
- Provide Visual Aids: When discussing medical information, using visual aids like diagrams or charts can assist patients in understanding complex concepts. Visual aids can be particularly helpful when language barriers exist.
What are the Potential Barriers to Effective Therapeutic Communication?
In the realm of healthcare, potential barriers to effective therapeutic communication are multifaceted. Lack of time is a common obstacle, as healthcare providers often have limited time to spend with each patient. This can lead to rushed communication and hinder the development of trust. Environmental factors, such as noise or interruptions in healthcare settings, can disrupt effective communication.
- Time Constraints: Healthcare professionals often work in fast-paced environments with limited time for each patient. Time constraints can hinder the thorough discussion of symptoms, treatment options, and patient concerns.
- Technology Dependence: Overreliance on technology, such as electronic health records, can create a barrier to communication. Healthcare providers may spend more time interacting with screens than with patients, reducing face-to-face communication.
- Lack of Training: Inadequate training in communication skills can be a significant barrier. Healthcare providers who have not received training on effective communication techniques may struggle to establish rapport with patients.
- Patient Fear and Anxiety: Patients experiencing fear or anxiety may have difficulty communicating their symptoms and concerns. These emotions can stem from the healthcare environment, medical procedures, or the severity of their condition.
- Stigma and Discrimination: Patients may fear being stigmatized or discriminated against due to their medical condition or personal characteristics. This fear can deter open and honest communication.
- Health Literacy: Limited health literacy can impede a patient’s ability to understand medical information and instructions. Healthcare providers should assess and address their patients’ health literacy levels to overcome this barrier.
Tips to Avoid Barriers of Therapeutic Communication in Nursing
Here are the Tips to Avoid Barriers of Therapeutic Communication in Nursing:
- Active Listening Techniques: Therapeutic communication in nursing hinges on active listening techniques that nurses can employ to foster a strong nurse-patient relationship. Nurses should focus on the patient’s verbal and nonverbal cues, allowing them to express their thoughts and feelings freely.
- Use of Open-Ended Questions: Using open-ended questions in nursing communication encourages patients to elaborate on their thoughts and concerns. These questions cannot be answered with a simple “yes” or “no” and require patients to provide more detailed responses.
- Nonverbal Communication Skills: Nonverbal cues play a significant role in therapeutic communication. Nurses should pay attention to their body language, facial expressions, and tone of voice. Maintaining eye contact, offering a comforting touch when appropriate, and using a warm tone can convey empathy and reassurance.
- Validation and Empathy: Validation and empathy are essential components of therapeutic communication. Validating a patient’s feelings and experiences demonstrates understanding and respect.
- Minimizing Jargon and Medical Terminology: Nurses should be cautious about using complex medical terminology and jargon when communicating with patients. Using language that is easily understandable to the patient ensures clarity and prevents misunderstandings.
Therapeutic communication in healthcare is vital for establishing trust and providing effective care. Recognizing and addressing barriers, employing communication techniques, and being aware of potential obstacles are essential steps for healthcare providers to enhance therapeutic communication with their patients. Effective therapeutic communication in nursing not only improves patient outcomes but also enhances the overall patient experience. By applying these tips and techniques, nurses can avoid communication barriers and foster a compassionate and trusting relationship with their patients.