19+ Communication Barriers Between Doctor and Patients Examples
Embark on a comprehensive journey exploring Communication Barriers Between Doctors and Patients. This H2 heading offers a succinct yet enlightening introduction, unraveling the intricacies that hinder effective medical communication. Delve into the guide to discover actionable solutions, illustrative Communication Examples, and insights to foster a more collaborative and understanding doctor-patient relationship. Enhance your healthcare interactions with practical tips for overcoming these barriers.
What is Communication Barriers Between Doctor and Patients?
In simple terms, Communication Barriers Between Doctors and Patients refer to obstacles hindering effective information exchange in the healthcare realm. This heading elucidates the complexities, providing a clear and straightforward definition for a better grasp of the dynamics surrounding communication challenges in the doctor-patient relationship.
What is the Best Example of Communication Barriers Between Doctor and Patients?
An illustrative example of communication barriers between doctors and patients involves prescription instructions. A doctor, using medical terminology, may unintentionally confuse the patient, leading to misunderstandings about medication dosage or usage. This H2 heading dissects this scenario, unraveling the intricacies and emphasizing the critical need for clear, patient-centric communication to enhance healthcare outcomes.
20 Communication Barriers Between Doctor and Patients Examples
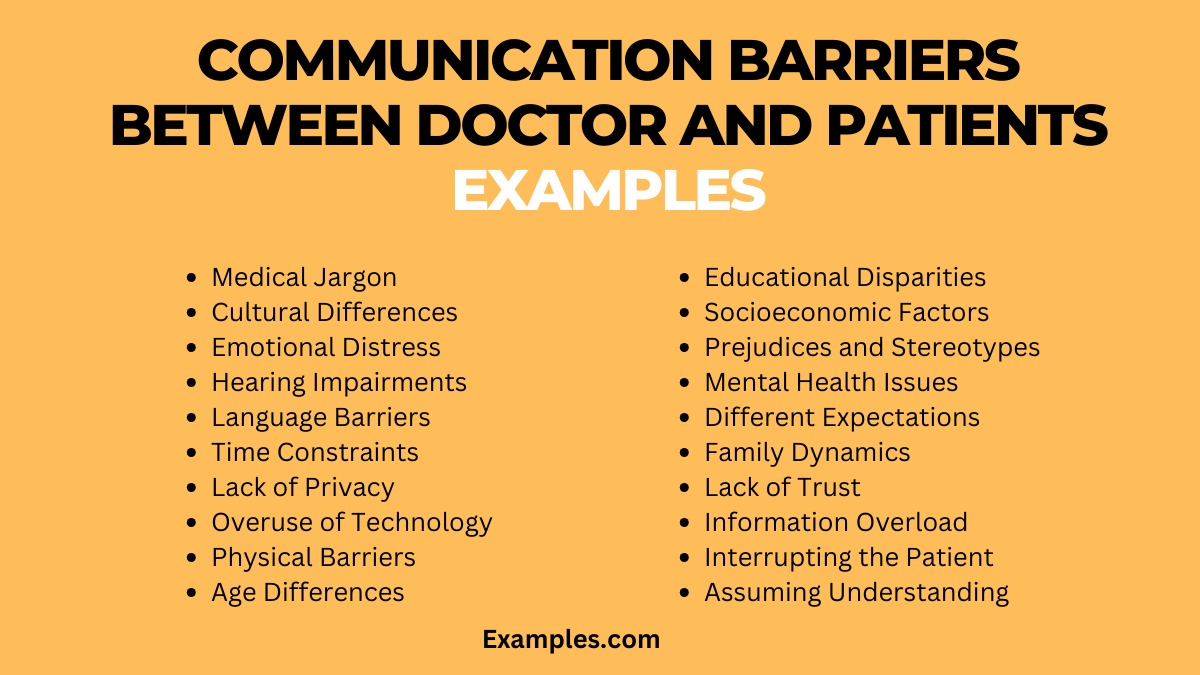
Misunderstandings between doctors and patients can lead to misdiagnosis, patient dissatisfaction, and poor treatment outcomes. This article delves into 20 common communication barriers and offers practical examples for overcoming them.
- Medical Jargon: Doctors often use technical language that patients don’t understand.
- “Instead of saying ‘benign neoplasm’, I’ll explain it as a ‘non-cancerous growth’.”
- Cultural Differences: Variations in cultural backgrounds can hinder understanding.
- “Could you share any cultural practices or beliefs that might impact your treatment?”
- Emotional Distress: Patients in distress might not comprehend information properly.
- “I know this is overwhelming. Let’s go through it step by step for clarity.”
- Hearing Impairments: Difficulty in hearing can impede effective communication.
- “Would you prefer written information or should we speak louder and more clearly?”
- Language Barriers: Non-native speakers may struggle to understand medical terms.
- “Is there a language you’re more comfortable communicating in?”
- Time Constraints: Rushed appointments can leave patients feeling unheard.
- “Even though our time is limited, I want to address your main concerns today.”
- Lack of Privacy: Discussing sensitive issues requires a private setting.
- “Let’s find a more private space to talk about this.”
- Overuse of Technology: Excessive reliance on technology can depersonalize communication.
- “Let me put aside the computer so we can talk more directly.”
- Physical Barriers: Physical distance or barriers in the consultation room.
- “Let’s sit closer so we can communicate more effectively.”
- Age Differences: Age-related factors can affect how information is received.
- “I’ll explain it in a way that’s easy for any age to understand.”
- Educational Disparities: Patients with different educational backgrounds may require simpler explanations.
- “Let me break down the treatment plan into simpler steps.”
- Socioeconomic Factors: Socioeconomic status can influence understanding and access to care.
- “Are there any financial constraints we should consider for your treatment?”
- Prejudices and Stereotypes: Unconscious biases can impact patient care.
- “I aim to treat all my patients with equal care and respect.”
- Mental Health Issues: Psychological conditions can complicate communication.
- “Let’s discuss how your mental health might be impacting your physical health.”
- Different Expectations: Misaligned expectations between doctor and patient.
- “Let’s set realistic goals and expectations for your treatment.”
- Family Dynamics: Family opinions and dynamics can influence patient decisions.
- “Would you like to involve your family in this discussion?”
- Lack of Trust: Distrust in the medical system or provider.
- “Building trust is important. Let’s address any concerns you have.”
- Information Overload: Too much information can overwhelm patients.
- “Let’s focus on the most critical information first.”
- Interrupting the Patient: Not allowing patients to fully express themselves.
- “Please take your time to explain; I’m here to listen.”
- Assuming Understanding: Assuming the patient understands without confirming.
- “Do you have any questions or need me to go over anything again?”
Communication Barriers Between Doctor and Patients in Hospital Examples
In hospitals, effective communication between doctors and patients is crucial for quality care. However, barriers like time constraints, environmental noise, and patient diversity pose challenges. Overcoming these can enhance understanding, trust, and treatment outcomes.
- Time Constraints: Doctors often face tight schedules, leading to brief patient interactions. To communicate better: “I want to address all your concerns, could you please prioritize your most pressing issues?”
- Environmental Noise: Hospitals are noisy, which can hinder clear conversations. To communicate better: “Let’s find a quieter spot for this discussion to ensure you understand everything clearly.”
- Patient Diversity: Varied backgrounds of patients require tailored communication strategies. To communicate better: “I’d like to understand your background better to communicate effectively with you.”
- Emotional Overload: Patients in hospitals often experience high stress. To communicate better: “I see this is overwhelming. Shall we go over this again when you feel more comfortable?”
- Physical Barriers: Equipment and bed arrangements can create distance. To communicate better: “I’ll come closer so we can talk more easily, is that alright?”
Communication Barriers Between Doctor and Patients in Healthcare Examples
In the broader healthcare setting, communication barriers impact patient satisfaction and care effectiveness. Challenges like varying health literacy, digital communication limits, and personal biases must be addressed for improved healthcare outcomes.
- Health Literacy Variance: Patients have different levels of health knowledge. To communicate better: “I’ll explain this in a way that’s easy to understand, regardless of your medical knowledge.”
- Digital Communication Gaps: Telehealth and emails can lack personal touch. To communicate better: “I want to ensure you feel heard even in our digital conversations.”
- Personal Biases: Unconscious biases from healthcare providers can affect interactions. To communicate better: “I strive to understand and respect all patients’ backgrounds and beliefs.”
- Complex Medical Terms: Overuse of medical jargon confuses patients. To communicate better: “Let me break down these terms into simpler language for clarity.”
- Patient Privacy Concerns: Concerns about confidentiality can inhibit open discussions. To communicate better: “Your privacy is paramount; feel safe to share your concerns.”
Which of the following is a barrier to communication between doctor and patients?
Effective communication between doctors and patients is essential for quality healthcare. However, several barriers can hinder this crucial interaction. Explore the following key obstacles that often impede the flow of information between medical professionals and individuals seeking care:
1. Language Disparities
Language differences can lead to misunderstandings, affecting the accurate exchange of medical information. Overcoming language barriers is crucial for ensuring patients comprehend diagnoses, treatments, and instructions.
2. Time Constraints
Limited consultation time can hinder in-depth discussions, leaving patients with unanswered questions and physicians with insufficient information about patient concerns.
3. Cultural Variations
Diverse cultural backgrounds may lead to varying communication styles and expectations, creating challenges in understanding and addressing healthcare needs.
4. Health Literacy Issues
Patients with limited health literacy may struggle to comprehend medical jargon and treatment plans, impacting their ability to actively participate in decision-making.
5. Emotional Barriers
Patient anxiety, fear, or emotional distress can interfere with effective communication, making it challenging for doctors to gather comprehensive medical histories and provide necessary support.
Understanding and addressing these barriers is pivotal for fostering improved doctor-patient communication, ultimately enhancing the overall quality of healthcare experiences.
What is the most important factor in effective communication between doctors and patients?
Empathy stands as the cornerstone of effective communication between doctors and patients. This essential factor transcends mere information exchange, creating a compassionate and understanding connection. When healthcare providers empathize with patients, they comprehend not only the medical aspects of their conditions but also the emotional and psychological dimensions.
Key Aspects of Empathetic Communication:
1. Active Listening
Empathetic doctors engage in active listening, attentively understanding patients’ concerns, fears, and expectations.
2. Understanding Patient Perspectives
By acknowledging and appreciating the unique perspectives and values of patients, doctors can tailor their communication to align with individual needs.
3. Clear and Compassionate Explanation
Empathetic communication involves clear and compassionate explanations of medical conditions, treatment plans, and potential outcomes, ensuring patients are well-informed.
4. Addressing Emotional Needs
Recognizing and addressing patients’ emotional needs fosters a supportive environment, enhancing overall patient satisfaction and treatment adherence.
5. Shared Decision-Making
Empathy facilitates collaborative decision-making, allowing patients to actively participate in their healthcare journey and contribute to treatment plans.
In conclusion, understanding and addressing communication barriers between doctors and patients is pivotal for optimal healthcare outcomes. By recognizing the impact of language disparities, lack of empathy, and information overload, healthcare providers can implement strategies to enhance communication. Embracing effective and empathetic communication ensures patients receive the care they deserve, fostering a collaborative and supportive healthcare environment.