Preparing for the NCLEX PN® Exam requires a thorough understanding of the gastrointestinal system and nutrition, essential components of nursing care. Mastery of digestive anatomy, nutrient absorption, and dietary needs is crucial. This knowledge aids in managing digestive disorders, providing nutritional support, and promoting overall gastrointestinal health, essential for patient well-being.
Learning Objective
In studying “Gastrointestinal/Nutrition” for the NCLEX PN® Exam, you should aim to understand the structure and function of the gastrointestinal tract, including the processes of digestion, absorption, and metabolism. Learn to identify common gastrointestinal disorders such as GERD, peptic ulcers, and inflammatory bowel disease, and their nutritional implications. Evaluate dietary needs, therapeutic diets, and nutritional support methods like enteral and parenteral nutrition. Additionally, explore the impact of nutrition on health and disease prevention, and apply this knowledge to develop effective nursing care plans that address patients’ dietary needs and promote gastrointestinal health.
Anatomy of the Gastrointestinal System
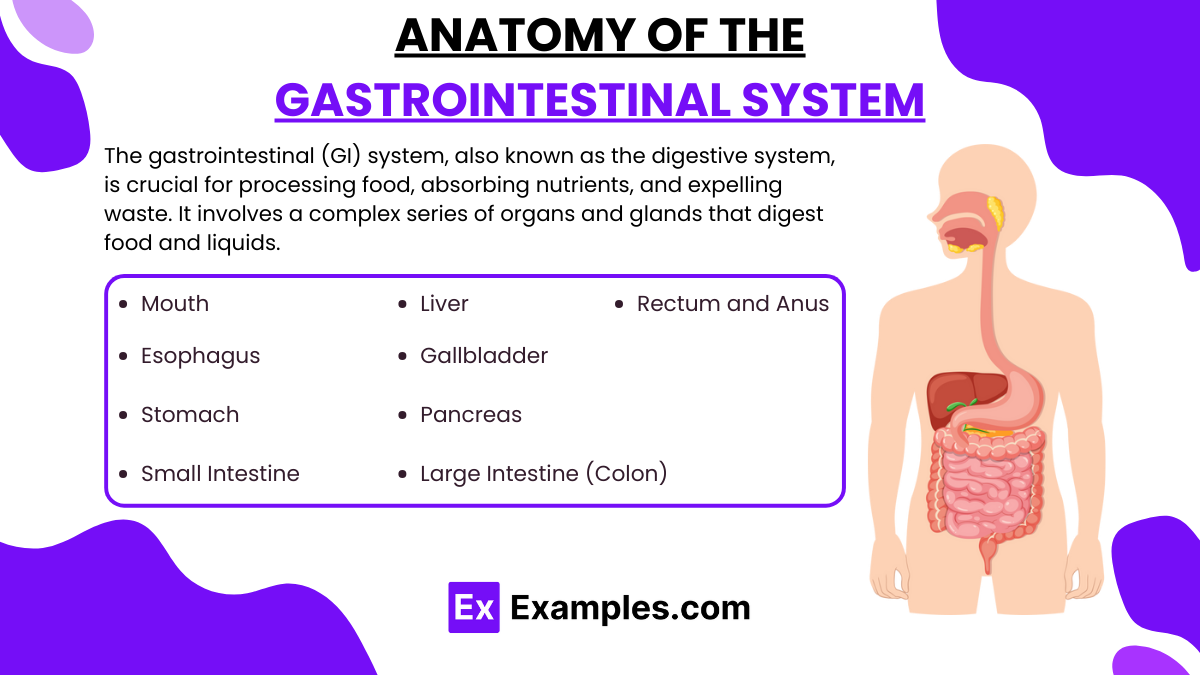
The gastrointestinal (GI) system, also known as the digestive system, is crucial for processing food, absorbing nutrients, and expelling waste. It involves a complex series of organs and glands that digest food and liquids. Here’s an overview of the anatomy of the gastrointestinal system:
- Mouth
- Function: Begins digestion by mechanically breaking down food through chewing and mixing it with saliva, which contains enzymes that start the breakdown of carbohydrates.
- Esophagus
- Function: A muscular tube that connects the throat (pharynx) with the stomach. The esophagus uses rhythmic, wave-like muscle movements called peristalsis to propel food to the stomach.
- Stomach
- Function: Continues the process of mechanical digestion; its glands produce stomach acid and enzymes that begin the digestion of proteins. The stomach also acts as a temporary storage tank for food, gradually releasing it into the small intestine.
- Small Intestine
- Function: Made up of three parts: the duodenum, jejunum, and ileum. The small intestine is the major site for digestion and absorption of nutrients. It receives digestive enzymes and bile to aid in digestion.
- Liver
- Function: Produces bile that is necessary for lipid digestion and absorption. It also processes nutrients absorbed from the small intestine.
- Gallbladder
- Function: Stores and concentrates bile, releasing it into the small intestine to aid in digestion when needed.
- Pancreas
- Function: Produces digestive enzymes and bicarbonate, which are delivered into the small intestine to aid in digestion and neutralize stomach acid.
- Large Intestine (Colon)
- Function: Absorbs water and salts from the material that has not been digested as food, and is thus involved in the formation of solid waste (feces). It also houses a large number of bacteria that play a role in the digestive process.
- Rectum and Anus
- Function: The rectum is the final section of the large intestine that terminates in the anus, where feces are expelled.
Nutritional Needs Across the Lifespan
Nutritional needs vary significantly throughout the human lifespan, influenced by growth, development, and changes in metabolism. Each life stage has distinct dietary requirements necessary for optimal health. Here’s an overview of nutritional needs across different stages of life:
1. Infancy (0-12 months)
- Nutrients: High needs for energy, protein, vitamins, and minerals per kilogram of body weight.
- Breastfeeding: Recommended exclusively for the first 6 months, providing ideal nutrition and protective antibodies.
- Solid Foods: Introduced around 6 months to complement breastfeeding and meet nutritional needs.
2. Childhood (1-12 years)
- Growth and Development: Nutrient-dense foods are essential for physical growth and cognitive development.
- Calcium and Vitamin D: Crucial for bone development.
- Iron: Important for cognitive development and preventing anemia.
3. Adolescence (13-18 years)
- Rapid Growth: Increased needs for energy, protein, calcium, and iron, especially for girls who begin menstruating.
- Calcium: Vital for final phases of bone growth.
- Healthy Habits: Establishing a healthy diet and physical activity routine to prevent obesity.
4. Adulthood (19-65 years)
- Maintenance: Focus on nutrients to maintain body repair, metabolism, and prevent chronic diseases.
- Caloric Needs: Vary based on activity level, with a gradual decrease in caloric needs with age.
- Fiber: Important for digestive health and preventing metabolic syndrome.
- Preventive Nutrition: Adequate intake of fruits, vegetables, whole grains, lean proteins, and healthy fats to mitigate risk of chronic diseases like type 2 diabetes, hypertension, and cardiovascular diseases.
5. Older Adults (65+ years)
- Decreased Caloric Needs: Due to a natural decline in basal metabolic rate and physical activity.
- Protein: Essential to reduce the loss of muscle mass.
- Calcium and Vitamin D: Important for bone health and to prevent osteoporosis.
- Vitamin B12: Absorption decreases with age; supplements or fortified foods might be necessary.
Role of the Nurse in Gastrointestinal/Nutritional Care
Nurses play a critical role in gastrointestinal and nutritional care across various healthcare settings, including hospitals, outpatient clinics, and community health centers. Their responsibilities encompass a wide range of activities, from assessing and monitoring patients to providing direct care and education. Here’s an overview of the specific roles and responsibilities of nurses in this specialized area of care:
1. Assessment and Monitoring
- Nutritional Assessment: Nurses perform nutritional screenings and assessments to identify patients at risk of malnutrition or those with existing nutritional deficiencies. This includes reviewing dietary intake, weight changes, body mass index (BMI), and relevant lab results.
- Gastrointestinal Symptoms: Nurses assess patients for symptoms related to gastrointestinal disorders, such as nausea, vomiting, diarrhea, constipation, and abdominal pain. They monitor the severity, frequency, and duration of these symptoms.
2. Direct Patient Care
- Feeding Assistance: Nurses may assist patients with eating difficulties, ensuring they receive adequate nutrition. This could involve positioning, help with utensils, or feeding patients directly if they are unable to do so themselves.
- Management of Feeding Tubes: For patients who cannot eat by mouth, nurses manage enteral feeding through tubes, such as nasogastric or gastrostomy tubes, ensuring proper placement, maintenance, and delivery of nutrition.
- Administration of Medications: Nurses administer medications that affect gastrointestinal function or are used to treat nutritional deficiencies. This includes administering IV fluids, electrolytes, and other supplements.
3. Patient Education
- Dietary Guidance: Nurses educate patients and their families on dietary modifications required for managing specific gastrointestinal conditions, like Crohn’s disease, ulcerative colitis, celiac disease, or irritable bowel syndrome.
- Nutritional Supplements: They provide information about the appropriate use of nutritional supplements to address deficiencies or support overall nutritional status.
- Lifestyle Modifications: Nurses advise on lifestyle changes that can improve gastrointestinal health and nutritional status, including physical activity, smoking cessation, and alcohol consumption.
4. Care Coordination
- Collaboration with Dietitians and Physicians: Nurses often collaborate with dietitians and physicians to create and implement comprehensive care plans tailored to the individual needs of patients.
- Referrals: They facilitate referrals to other healthcare professionals as needed for further assessment, counseling, or specialized care.
5. Support and Advocacy
- Emotional Support: Providing emotional and psychological support is a key aspect of nursing, particularly for patients dealing with chronic gastrointestinal issues which can significantly affect quality of life.
- Advocacy: Nurses advocate for their patients’ healthcare needs, ensuring they receive appropriate and timely interventions.
6. Monitoring and Managing Complications
- Complication Prevention: Nurses monitor patients for potential complications arising from nutritional deficiencies or gastrointestinal disorders, such as dehydration, electrolyte imbalances, or bowel obstructions.
- Response to Acute Situations: They are often the first to respond to acute situations like gastrointestinal bleeding or severe dehydration, initiating necessary interventions and notifying physicians.
Examples
Example 1: Managing GERD
- A patient with chronic gastroesophageal reflux disease (GERD) needs dietary and lifestyle modifications. The nurse advises avoiding large, fatty meals and late-night eating, elevating the head of the bed, and avoiding caffeine and alcohol. The patient is also educated on the importance of taking prescribed proton pump inhibitors correctly.
Example 2: Dietary Adjustments for Peptic Ulcer Disease
- A patient diagnosed with peptic ulcer disease due to Helicobacter pylori infection is advised on appropriate dietary changes. The nurse suggests avoiding spicy foods, alcohol, and smoking. The patient is taught how these factors exacerbate symptoms and is instructed on the correct use of prescribed antibiotics and antacids.
Example 3: Nutritional Support for Crohn’s Disease
- For a patient with Crohn’s disease experiencing a flare-up, the nurse coordinates with a dietitian to adjust the patient’s diet to include low-residue, high-protein, and high-calorie foods to minimize intestinal irritation and meet nutritional needs. Supplemental vitamins and minerals are administered to counteract malabsorption.
Example 4: Enteral Feeding in Pancreatitis
- A patient with acute pancreatitis is unable to consume food orally. The nurse manages the administration of enteral nutrition through a nasogastric tube, ensuring the patient receives adequate nutrients while resting the pancreas. The nurse monitors for complications such as aspiration and tube displacement.
Example 5: Nutritional Counseling for Liver Cirrhosis
- In managing a patient with liver cirrhosis, the nurse emphasizes the importance of a low-sodium diet to prevent fluid accumulation leading to ascites. Nutritional education also includes the need to limit protein intake to prevent hepatic encephalopathy. The nurse arranges for periodic nutritional assessments to adjust the diet as needed.
Practice Questions
Question 1
A patient with dehydration exhibits which of the following symptoms primarily?
A. Edema
B. Hypertension
C. Tachycardia
D. Bradycardia
Answer:
C. Tachycardia
Explanation:
Dehydration often leads to decreased blood volume, prompting compensatory mechanisms such as tachycardia to maintain cardiac output and blood pressure. Edema (option A) and hypertension (option B) are typically associated with fluid overload, not dehydration. Bradycardia (option D) is generally not a primary symptom of dehydration and would be more related to other clinical scenarios.
Question 2
Which acid-base imbalance is characterized by an elevated blood pH and a bicarbonate level higher than normal?
A. Respiratory acidosis
B. Metabolic acidosis
C. Respiratory alkalosis
D. Metabolic alkalosis
Answer:
D. Metabolic alkalosis
Explanation:
Metabolic alkalosis occurs when there is an accumulation of bicarbonate or a loss of hydrogen ions, which leads to an increase in blood pH. Respiratory acidosis (option A) and metabolic acidosis (option B) are both characterized by a lower blood pH. Respiratory alkalosis (option C) involves an elevated pH but is typically due to excessive exhalation of CO2 rather than changes in bicarbonate levels.
Question 3
Which electrolyte imbalance is commonly associated with muscle twitching and convulsions?
A. Hyperkalemia
B. Hypokalemia
C. Hyponatremia
D. Hypocalcemia
Answer:
D. Hypocalcemia
Explanation:
Hypocalcemia, or low calcium levels in the blood, can lead to increased neuromuscular excitability, resulting in symptoms such as muscle twitching, cramping, and convulsions. Hyperkalemia (option A) and hypokalemia (option B) primarily affect cardiac function and muscle strength, whereas hyponatremia (option C) typically impacts brain function, potentially leading to confusion and seizures in severe cases.