The “Maternal & Newborn Health: Reproductive” section of the NCLEX-RN® exam focuses on the comprehensive care of women during pregnancy, childbirth, and the postpartum period, as well as newborn care. It evaluates a nurse’s ability to provide safe, effective care, emphasizing reproductive anatomy, prenatal care, labor and delivery, and postpartum management. Nurses must demonstrate knowledge of maternal and neonatal complications, nursing interventions, and patient education. Mastery of this area is crucial for ensuring positive maternal and newborn outcomes and achieving a high score on the NCLEX-RN®.
Learning Objectives
In studying “Maternal & Newborn Health: Reproductive” for the NCLEX-RN® exam, you should learn to understand key concepts related to reproductive health, pregnancy, labor, delivery, and postpartum care. Analyze the physiological changes during pregnancy, stages of labor, and common maternal and newborn complications. Evaluate nursing interventions for prenatal care, labor support, and postpartum recovery. Additionally, explore maternal mental health issues, breastfeeding techniques, and newborn assessments, including APGAR scoring and reflex evaluation. Apply your understanding to interpret clinical scenarios, prioritize nursing actions, and provide safe, evidence-based care for maternal and newborn patients in NCLEX-style questions and practice passages
1. Reproductive Anatomy & Physiology
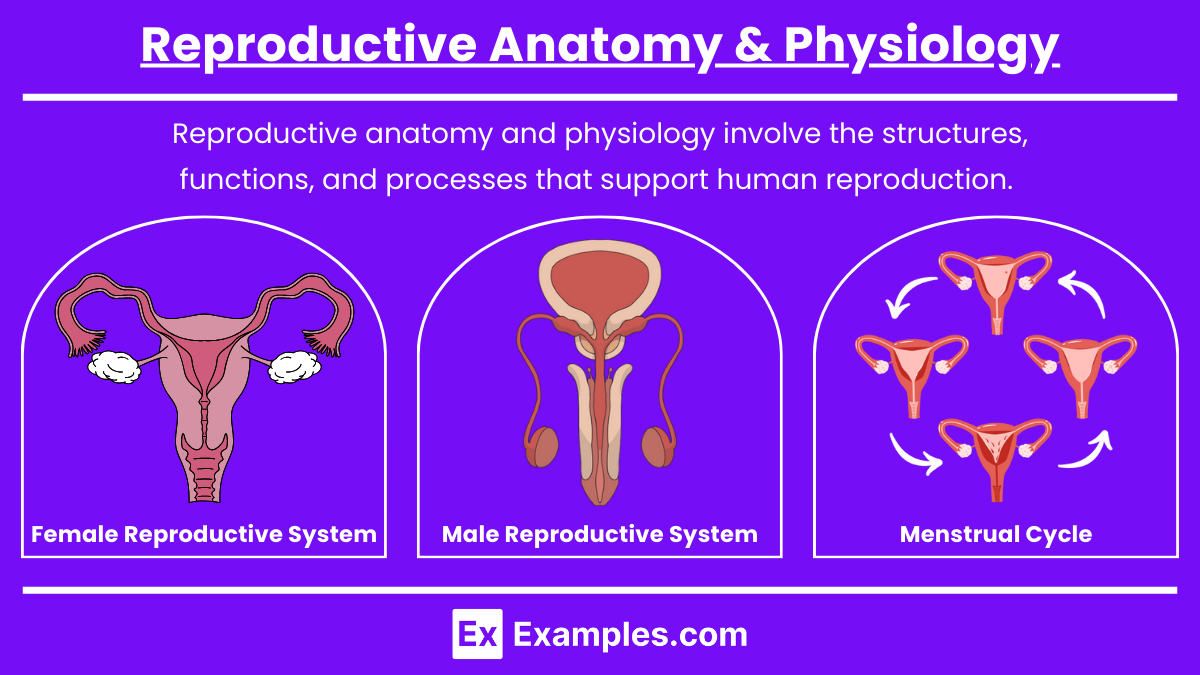
Reproductive anatomy and physiology involve the structures, functions, and processes that support human reproduction. This includes the male and female reproductive systems, hormonal regulation, and the menstrual cycle, all of which are critical for conception, pregnancy, and childbirth.
Key Concepts
1.Female Reproductive System
- External Structures: Labia majora, labia minora, clitoris, vestibule, Bartholin’s glands.
- Function: Protect internal structures, provide sexual arousal, and facilitate lubrication.
- Internal Structures: Vagina, cervix, uterus, fallopian tubes, and ovaries.
- Vagina: Birth canal and pathway for menstrual flow.
- Uterus: Site for implantation, fetal development, and contractions during labor.
- Ovaries: Produce ova (eggs) and secrete estrogen and progesterone.
- Fallopian Tubes: Site for fertilization, connecting ovaries to the uterus.
2.Male Reproductive System
- Structures: Testes, epididymis, vas deferens, seminal vesicles, prostate gland, penis.
- Testes: Produce sperm and testosterone.
- Epididymis: Maturation and storage of sperm.
- Vas Deferens: Transports sperm from the epididymis to the urethra.
3.Menstrual Cycle
- Phases:
- Menstrual Phase (1-5 days): Shedding of the endometrial lining.
- Follicular Phase (6-13 days): FSH stimulates follicle development; estrogen increases.
- Ovulation (Day 14): LH surge triggers the release of an egg from the ovary.
- Luteal Phase (15-28 days): Corpus luteum secretes progesterone; endometrium thickens.
- Hormonal Regulation: FSH, LH, estrogen, and progesterone work in a cycle to promote ovulation and maintain pregnancy.
2. Pregnancy & Prenatal Care
Pregnancy and prenatal care focus on the period from conception to birth. Prenatal care ensures the health of the mother and fetus through medical checkups, screening tests, and lifestyle education to reduce risks and detect complications early.
Key Concepts
Preconception Health
- Definition: Care provided before pregnancy to improve maternal health and reduce pregnancy risks.
- Interventions:
- Folic acid supplementation (400-800 mcg/day) to prevent neural tube defects.
- Lifestyle changes: Avoid smoking, alcohol, and drug use.
- Screenings for chronic diseases (diabetes, hypertension) and STIs.
Prenatal Care
- Initial Prenatal Visit:
- Health History: Obstetric history (GTPAL system), current health status, and family history.
- Lab Tests: CBC, blood type and Rh, rubella immunity, HIV, STIs, glucose screening, and urinalysis.
- Education: Importance of prenatal vitamins, nutrition, and lifestyle changes.
- Ongoing Prenatal Visits:
- Visit schedule: Every 4 weeks (0-28 weeks), every 2 weeks (28-36 weeks), weekly (36 weeks until delivery).
- Key assessments: Weight, blood pressure, fundal height, fetal heart rate, and glucose tolerance test at 24-28 weeks.
Pregnancy Stages
- First Trimester (Weeks 1-12):
- Symptoms: Nausea, vomiting, fatigue, breast tenderness.
- Complications: Miscarriage, ectopic pregnancy.
- Second Trimester (Weeks 13-26):
- Symptoms: Quickening (fetal movement), improved energy, and decreased nausea.
- Complications: Gestational diabetes, preeclampsia, preterm labor.
- Third Trimester (Weeks 27-40):
- Symptoms: Braxton Hicks contractions, back pain, and increased urinary frequency.
- Complications: Placenta previa, placental abruption, and oligohydramnios.
3. Labor, Delivery & Postpartum Care
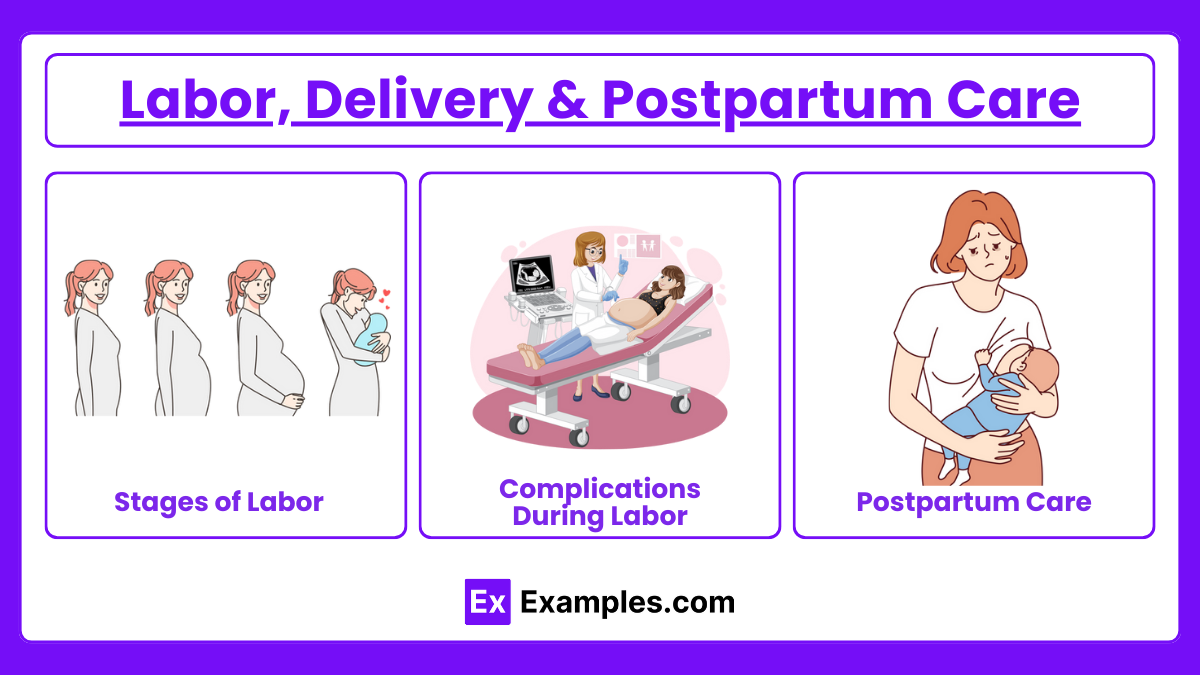
Labor, delivery, and postpartum care encompass the stages of childbirth and the mother’s physical and emotional recovery after birth. The focus is on ensuring safe delivery and preventing complications such as hemorrhage, infection, or postpartum depression.
Key Concepts
Stages of Labor
- Stage 1 (Dilation)
- Latent Phase (0-3 cm): Slow dilation, mild contractions.
- Active Phase (4-7 cm): Stronger contractions; pain management may be initiated.
- Transition Phase (8-10 cm): Strong contractions, intense pain, and maternal focus.
- Stage 2 (Delivery of Baby)
- Begins at full dilation (10 cm) and ends with the delivery of the baby.
- Stage 3 (Delivery of Placenta)
- Delivery of the placenta occurs 5-30 minutes after childbirth.
- Monitor for hemorrhage.
- Stage 4 (Recovery)
- First 1-2 hours after delivery.
- Nursing care: Monitor vital signs, assess fundus, and observe for bleeding.
Complications During Labor
- Prolapsed Cord: Umbilical cord drops ahead of the baby, requiring emergency intervention (knee-chest position).
- Shoulder Dystocia: Baby’s shoulder gets stuck during delivery, requiring maneuvers (McRoberts position).
- Preterm Labor: Use of tocolytics (like magnesium sulfate) to delay delivery.
Postpartum Care
- Uterine Involution: Return of the uterus to a pre-pregnancy state.
- Postpartum Hemorrhage: Blood loss >500 mL (vaginal) or >1000 mL (cesarean).
- Mental Health:
- Baby Blues: Emotional changes, resolve within 2 weeks.
- Postpartum Depression: Lasts longer than 2 weeks, requires treatment.
- Postpartum Psychosis: Emergency requiring immediate intervention.
4. Newborn Care & Family Planning
Newborn care focuses on the immediate needs of the newborn, including assessment, screening, and health promotion. Family planning includes methods to prevent, delay, or achieve pregnancy through various contraception techniques.
Key Concepts
Newborn Assessment
- APGAR Score: Evaluated at 1 and 5 minutes, scoring 0-2 in each category (Appearance, Pulse, Grimace, Activity, Respiration).
- Physical Exam: Weight, length, head circumference, and assessment of reflexes (Moro, rooting, sucking).
- Newborn Reflexes:
- Rooting: Baby turns head toward touch on the cheek.
- Moro Reflex: Sudden extension of arms/legs when startled.
Newborn Screening & Medications
- Screenings: Metabolic screening, hearing tests, and bilirubin levels.
- Medications:
- Erythromycin Eye Ointment: Prevents eye infections.
- Vitamin K Injection: Prevents bleeding disorders.
- Hepatitis B Vaccine: Prevents hepatitis B infection.
Breastfeeding & Lactation
- Hormones:
- Prolactin: Stimulates milk production.
- Oxytocin: Causes milk ejection (let-down reflex).
- Breastfeeding Positions: Cradle, cross-cradle, football hold, and side-lying.
- Common Issues: Mastitis, nipple soreness, and engorgement.
Contraception & Family Planning
- Natural Methods: Abstinence, fertility awareness methods (basal body temperature, cervical mucus).
- Barrier Methods: Condoms, diaphragms, cervical caps.
- Hormonal Methods:
- Oral Contraceptives: Combined estrogen and progesterone pills.
- Emergency Contraception: Taken within 72 hours after unprotected sex.
- Intrauterine Device (IUD): Copper or hormonal IUDs, effective for 3-10 years.
- Permanent Methods:
- Tubal Ligation: Female sterilization.
- Vasectomy: Male sterilization.
Examples
Example 1: Nursing Care for a Patient with Preeclampsia
Preeclampsia is a hypertensive disorder that occurs during pregnancy and poses significant health risks for both the mother and the fetus. On the NCLEX-RN®, you may encounter questions where you must identify signs of preeclampsia, such as elevated blood pressure, proteinuria, and visual disturbances. The nurse’s role involves monitoring the patient’s blood pressure, assessing for signs of eclampsia (seizures), and administering medications like magnesium sulfate to prevent seizures. Nurses must also provide patient education on warning signs and promote a calm, low-stimulation environment. Priority interventions focus on preventing complications like placental abruption or fetal distress.
Example 2: Management of Preterm Labor
Preterm labor occurs when a pregnant woman begins labor contractions before 37 weeks of gestation. NCLEX-RN® questions may assess a nurse’s ability to recognize the signs of preterm labor, such as regular uterine contractions, cervical changes, or back pain. The nurse must initiate immediate interventions, which include administering tocolytic medications (like magnesium sulfate) to halt contractions and administering corticosteroids (like betamethasone) to accelerate fetal lung maturity. Nurses also provide patient education on signs of preterm labor, such as pelvic pressure and increased vaginal discharge, so the patient knows when to seek medical attention.
Example 3: Nursing Assessment and Care During Labor and Delivery
Labor and delivery are crucial moments in maternal and newborn health, and nurses play a vital role in ensuring the safety of the mother and baby. During labor, NCLEX-RN® scenarios may require nurses to assess the progress of labor using cervical dilation, effacement, and fetal station. Nurses must monitor the fetal heart rate (FHR) and recognize abnormal patterns, such as late decelerations, which indicate fetal distress. Interventions may include repositioning the patient, administering oxygen, and notifying the healthcare provider. Nurses also support the mother emotionally and physically during each phase of labor (latent, active, and transition), providing pain relief options and encouraging effective breathing techniques.
Example 4: Care for a Newborn with Jaundice
Newborn jaundice is a common issue that occurs due to elevated bilirubin levels in the baby’s blood, leading to yellowing of the skin and eyes. The NCLEX-RN® may present questions on recognizing signs of jaundice and selecting appropriate nursing interventions. Nurses should assess for jaundice by applying gentle pressure on the newborn’s skin to observe for yellowing. Management includes phototherapy, where the infant is placed under special blue lights that help break down excess bilirubin. Nurses must ensure the infant’s eyes are protected with eye shields and encourage frequent breastfeeding to promote bilirubin excretion through stool. Patient education on the signs of worsening jaundice and when to seek medical attention is also crucial.
Example 5: Postpartum Hemorrhage and Nursing Interventions
Postpartum hemorrhage (PPH) is a life-threatening condition defined as blood loss exceeding 500 mL after a vaginal birth or 1000 mL after a cesarean birth. NCLEX-RN® questions on PPH may require the nurse to prioritize care, which includes recognizing early signs of excessive bleeding, such as uterine atony (a boggy uterus), tachycardia, and low blood pressure. Nurses must perform uterine fundal massage to stimulate uterine contractions and prevent further bleeding. If this is ineffective, medications like oxytocin, misoprostol, or methylergonovine may be administered. Nurses also monitor for signs of hypovolemic shock, ensure accurate intake and output, and provide emotional support to the patient and family. Recognizing and addressing PPH quickly can be life-saving for the mother.
Practice Questions
Question 1
A 28-year-old woman at 34 weeks gestation arrives at the labor and delivery unit with complaints of a severe headache, blurred vision, and swelling of her hands and face. Upon assessment, her blood pressure is 170/110 mmHg, and a urine dipstick reveals 2+ proteinuria. Which of the following actions should the nurse prioritize?
A) Administer magnesium sulfate as prescribed
B) Place the client in a high-Fowler’s position
C) Administer hydralazine to reduce blood pressure
D) Encourage ambulation to improve circulation
Answer: A) Administer magnesium sulfate as prescribed
Explanation:
This client is showing signs of severe preeclampsia, a hypertensive disorder during pregnancy. The classic symptoms of severe preeclampsia include:
- Hypertension (BP ≥ 160/110 mmHg)
- Proteinuria (≥ 2+ on dipstick)
- Headache
- Blurred vision
- Edema (face, hands, feet)
The administration of magnesium sulfate is essential because it prevents seizures, which is a hallmark complication of severe preeclampsia (known as eclampsia). Magnesium sulfate acts as a central nervous system depressant to reduce the risk of seizures.
- Option B: Place the client in a high-Fowler’s position — This position is not appropriate for preeclampsia. While semi-Fowler’s may help with breathing, it does not address the risk of seizures.
- Option C: Administer hydralazine to reduce blood pressure — While hydralazine may be used to manage blood pressure in preeclampsia, preventing seizures takes priority. Magnesium sulfate addresses both seizure prevention and provides neuroprotection.
- Option D: Encourage ambulation to improve circulation — Ambulation is contraindicated in severe preeclampsia due to the risk of seizures, falls, and complications like placental abruption. The client should be placed on bed rest with seizure precautions.
Question 2
The nurse is caring for a 2-hour-old newborn. The nurse notes the baby has a bluish discoloration of the hands and feet but is otherwise pink and has a strong cry. What is the most appropriate nursing intervention?
A) Administer oxygen to the newborn
B) Notify the healthcare provider
C) Document the finding as normal
D) Place the newborn under a radiant warmer
Answer: C) Document the finding as normal
Explanation:
The bluish discoloration of the hands and feet in a newborn is called acrocyanosis, and it is a normal finding in newborns during the first 24 to 48 hours after birth. It occurs because of immature peripheral circulation, which prioritizes blood flow to vital organs (brain, heart, and lungs).
- Option A: Administer oxygen to the newborn — Oxygen administration is not necessary in acrocyanosis as it is a normal physiological response. Oxygen would be required in the case of central cyanosis, where the lips, tongue, and trunk are blue.
- Option B: Notify the healthcare provider — There is no need to notify the provider as this is a normal finding. Central cyanosis (bluish discoloration of the tongue, lips, and chest) would require immediate notification.
- Option D: Place the newborn under a radiant warmer — This intervention is done if the newborn is hypothermic. Acrocyanosis is not an indicator of hypothermia and does not require the use of a radiant warmer.
Question 3
A nurse is assessing a client at 39 weeks gestation who is in active labor. The fetal heart rate (FHR) shows late decelerations on the monitor. Which of the following nursing interventions should be the nurse’s priority?
A) Administer oxygen via face mask
B) Turn the client to her left side
C) Increase the rate of the intravenous (IV) infusion
D) Call the healthcare provider immediately
Answer: B) Turn the client to her left side
Explanation:
Late decelerations on the fetal heart rate (FHR) tracing are associated with uteroplacental insufficiency, meaning that the placenta is not delivering enough oxygen to the fetus. This can be caused by conditions like maternal hypotension, uterine hyperstimulation, or placental abruption.
The priority action is to improve uteroplacental perfusion, which can be done by turning the client to her left side. This position takes pressure off the inferior vena cava, improving blood flow to the placenta and oxygen delivery to the fetus.
- Option A: Administer oxygen via face mask — While oxygen can be useful, it is not the priority. Repositioning the client (Option B) improves perfusion faster and more effectively. Oxygen can be applied after repositioning if the FHR does not improve.
- Option C: Increase the rate of the intravenous (IV) infusion — Increasing fluids can improve perfusion, but repositioning comes first. After repositioning, increasing the IV rate may be appropriate, but it is not the initial intervention.
- Option D: Call the healthcare provider immediately — Calling the provider is not the priority. Nurses must use immediate interventions (like repositioning) to resolve the issue before escalation. Provider notification occurs only if interventions fail.


