What type of cells are primarily involved in cell-mediated immunity?
B cells
T cells
Macrophages
Antibodies

Cell-mediated immunity represents a vital aspect of the adaptive immune system, primarily involving T cells that directly attack and destroy infected or dysfunctional cells. This branch of immunity does not rely on antibodies but instead employs T cells to identify and eliminate cells harboring intracellular pathogens like viruses or certain bacteria. Essential for combating diseases where pathogens reside within cells, cell-mediated immunity also plays a crucial role in tumor suppression and transplant rejection, highlighting its importance in maintaining robust immune health and preventing disease.
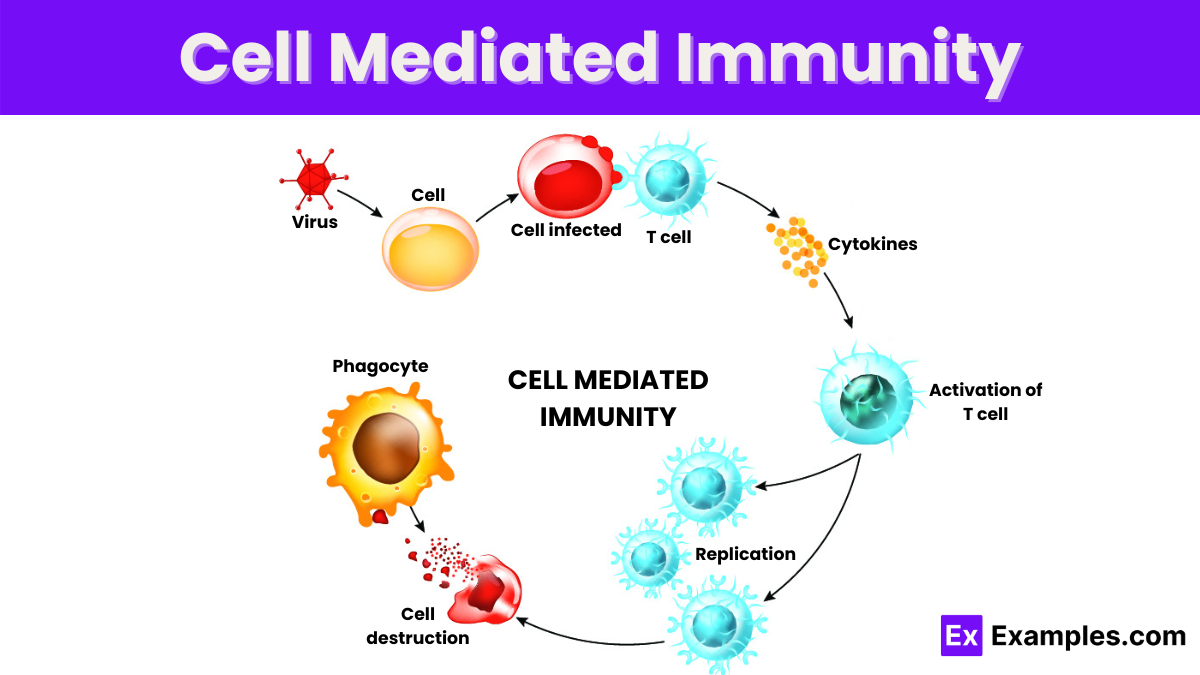
Cell-mediated immunity refers to an immune response that does not involve antibodies but rather involves the activation of phagocytes, antigen-specific cytotoxic T-lymphocytes, and the release of various cytokines in response to an antigen. This type of immunity is primarily mediated by T cells and is crucial for defending the body against pathogens that survive inside cells, such as viruses, some bacteria, and cancer cells. Cell-mediated immunity plays a vital role in recognizing and eliminating cells infected by pathogens, as well as tumor cells, through direct cell-to-cell contact and the release of cytokines, which are signaling molecules that aid in the immune response.
Cell-mediated immunity is essential for controlling infections by intracellular pathogens, such as viruses and some bacteria, which hide inside the cells where antibodies cannot reach them. It is also crucial in tumor suppression and plays a significant role in the rejection of transplanted organs, as the immune system recognizes the transplanted tissue as foreign.
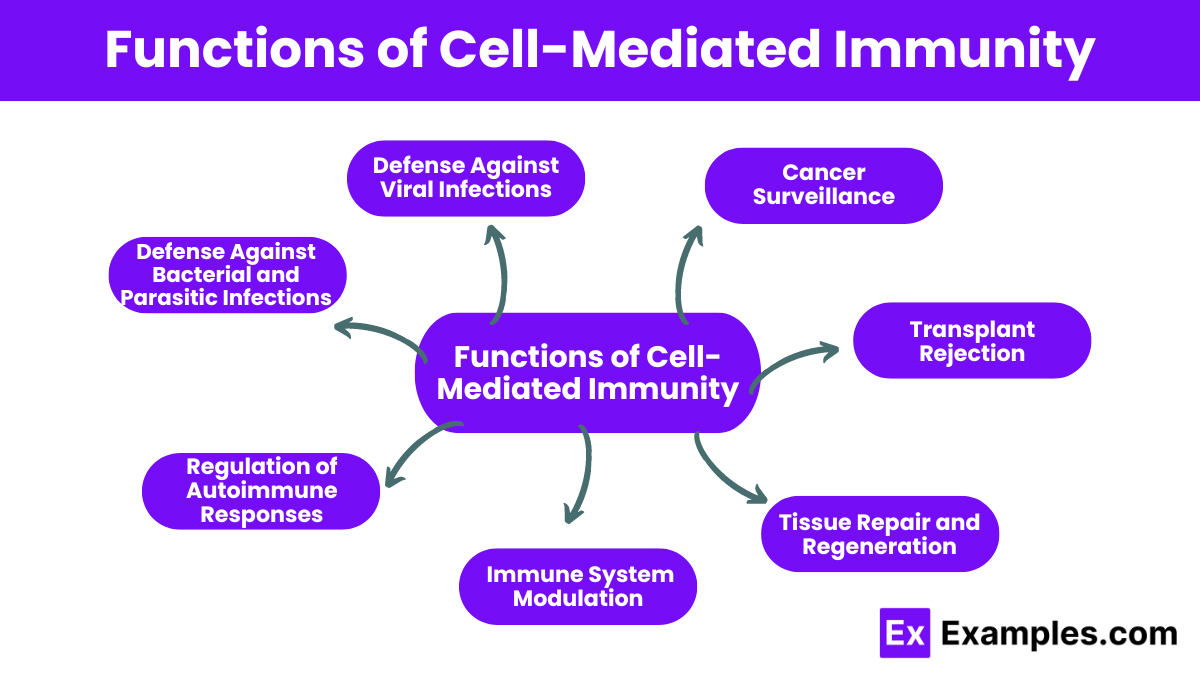
Cell-mediated immunity specifically targets and destroys cells infected by viruses, preventing the spread of the virus within the body.
It is crucial for eliminating intracellular bacteria and parasites that evade other components of the immune system by hiding within cells.
Cell-mediated immunity plays a key role in identifying and destroying cells that have undergone malignant transformation, thereby preventing the development and spread of cancer.
This function involves recognizing and attacking transplanted organs or tissues that do not match genetically, leading to rejection.
Regulatory T cells within the cell-mediated immune response help prevent autoimmune diseases by maintaining tolerance to the body’s own antigens and suppressing excessive immune responses.
Cell-mediated immunity modulates the overall immune response by activating and directing other immune cells through the secretion of cytokines and other signaling molecules.
Beyond its defensive roles, cell-mediated immunity also contributes to tissue repair and regeneration by orchestrating the removal of dead cells and supporting the renewal of tissues after an immune response or injury.
Cytotoxic T cells (CTLs) or CD8+ T cells are perhaps the most critical players in cell-mediated immunity. These cells recognize and destroy infected cells, cancer cells, and cells of transplanted tissues. They are particularly effective against viral infections. The process involves CTLs recognizing foreign or abnormal peptides presented by MHC class I molecules on the surface of infected cells. Once engaged, CTLs release perforins and granzymes, which induce apoptosis in the target cell, effectively eliminating the threat.
Helper T cells, or CD4+ T cells, do not directly kill infected cells. Instead, they support other cells in the immune system through the secretion of cytokines, which enhance the response of B cells (for antibody production), cytotoxic T cells, and macrophages. Helper T cells are crucial in both cell-mediated and humoral immune responses and are subdivided into various types, including Th1, Th2, Th17, and Treg cells, each with distinct functions and cytokine profiles.
Delayed-type hypersensitivity is a type of immune response mediated by T cells, which occurs several hours to days after exposure to the antigen. It is typically seen in response to bacterial infections, fungal infections, and contact allergens (like poison ivy or nickel). In DTH, activated Th1 cells release cytokines that recruit and activate macrophages. The macrophages increase in size and number, leading to inflammation and tissue damage at the site of antigen exposure.
While NK cells are part of the innate immune system, their functions overlap significantly with cell-mediated immunity. NK cells can kill virus-infected cells and tumor cells without prior sensitization, which distinguishes them from cytotoxic T cells that require activation. NK cells detect stressed cells in the absence of MHC (missing self) and kill these cells by releasing cytotoxic granules.
Macrophages are versatile cells involved in both innate and adaptive immunity. In cell-mediated immunity, macrophages are activated by cytokines produced by helper T cells (especially Th1 cells). Once activated, macrophages become highly phagocytic and produce various cytotoxic substances that are effective against bacteria, fungi, and tumor cells. They also play a crucial role in antigen presentation and cytokine production, further promoting the immune response.
Cell-mediated immunity involves several key components that work together to defend the body against pathogens that are not accessible by antibodies alone. Here are the primary elements of this critical immune response system:
T cells are the central figures in cell-mediated immunity. They originate in the bone marrow and mature in the thymus. There are several types of T cells, each serving a distinct function:
APCs, including dendritic cells, macrophages, and B cells, play a crucial role in the immune response. They capture antigens, process them, and present them on their surface in a form that T cells can recognize. This process is vital for the activation of T cells.
MHC molecules are essential for immune function. They are cell surface proteins that display bits of processed antigen to T cells. There are two classes of MHC molecules:
Cytokines are signaling molecules that mediate and regulate immunity, inflammation, and hematopoiesis. In cell-mediated immunity, cytokines direct the immune response by signaling between the cells of the immune system, helping to activate or suppress various immune responses.
Although not T cells, NK cells are included in cell-mediated immunity because they play a similar role to cytotoxic T cells but do not require antigen stimulation to kill. NK cells target and destroy virally infected cells and cancer cells through mechanisms that do not always require MHC presentation.
Cell-mediated immunity is exemplified by the body’s response to the Varicella zoster virus, which causes chickenpox. Initially, when the virus infects cells, it is recognized by cytotoxic T cells (CD8+ T cells), which are activated to destroy virus-infected cells, limiting the virus’s spread. Concurrently, helper T cells (CD4+ T cells) are activated by antigen-presenting cells and help by producing cytokines that boost cytotoxic T cell function and stimulate antibody production by B cells. After the infection, memory T cells are formed, providing long-lasting immunity and a rapid response to future exposures. This response showcases the crucial role of cell-mediated immunity in fighting viral infections and forming the basis for vaccines like those against chickenpox and shingles.
T-cells attacking infected cells directly is a prime example of a cell-mediated immune response, crucial for targeting viruses and cancer cells.
Humoral immunity uses antibodies in body fluids, while cell-mediated immunity involves T-cells that directly attack pathogens.
Cell-mediated immunity is essential for protecting against viruses, fungi, and some bacteria, and plays a key role in tumor surveillance.
Cell-mediated immunity is a part of the adaptive immune system, involving specialized cells that learn to recognize specific pathogens.
Cell-mediated immunity is adaptive as it develops memory of specific pathogens, enabling a faster response on subsequent exposures.
Text prompt
Add Tone
10 Examples of Public speaking
20 Examples of Gas lighting
What type of cells are primarily involved in cell-mediated immunity?
B cells
T cells
Macrophages
Antibodies
Which of the following describes the role of helper T cells in cell-mediated immunity?
They directly kill infected cells
They activate other immune cells
They produce antibodies
They remove dead cells
What is the primary function of cytotoxic T cells?
To produce antibodies
To help B cells
To destroy infected or cancerous cells
To secrete cytokines
What is the significance of antigen presenting cells (APCs) in cell-mediated immunity?
They produce antibodies
They present antigens to T ce
They engulf pathogens
They generate memory cells
Which of the following best describes the process of clonal selection in T cells?
All T cells respond equally
Specific T cells are activated and proliferate in response to an antigen
T cells create antibodies
T cells become memory cells without activation
Which cytokine is most important for the proliferation and activation of T cells?
Interleukin-1
Interferon-gamma
Interleukin-2
Tumor necrosis factor
What is the role of memory T cells in the immune response?
They are involved in the immediate response to infection
They help B cells produce antibodies
They provide a faster and stronger response upon re-exposure to the same antigen
They destroy pathogens directly
Which of the following is a characteristic of cell-mediated immunity compared to humoral immunity?
Involves B cells and antibodies
Targets extracellular pathogens
Involves direct attack on infected cells
Relies on memory cells for antibody production
What is the main purpose of using vaccines in relation to cell-mediated immunity?
To enhance antibody production
To create memory T and B cells
To provide immediate immunity
To activate phagocytes
How do perforins and granzymes function in the immune response?
They help in the activation of B cells
They produce antibodies
They induce apoptosis in target cells
They present antigens to T cells
Before you leave, take our quick quiz to enhance your learning!

