3+ Soap Note Assessment Examples to Download
In the medical or healthcare field, it is always a requirement to make your notes as concise, clear and hit the target as possible. This way, when it is time to make some assessments or notes, it would be easier and clearer to understand. In addition to that, it would also take less time to understand the situation and to find a solution through notes. SOAP notes are easy to make if you know what they mean and how to use them. To know more about SOAP note assessments, check out the article below.
3+ Soap Note Assessment Examples
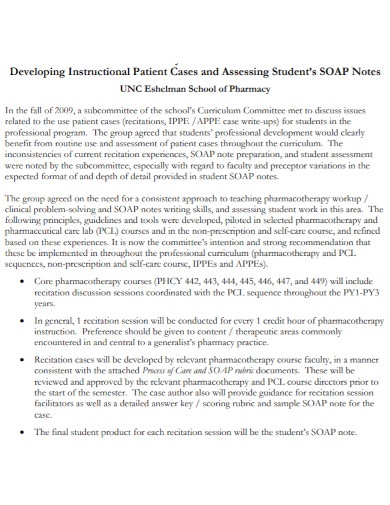
1. Student Soap Note Assessment
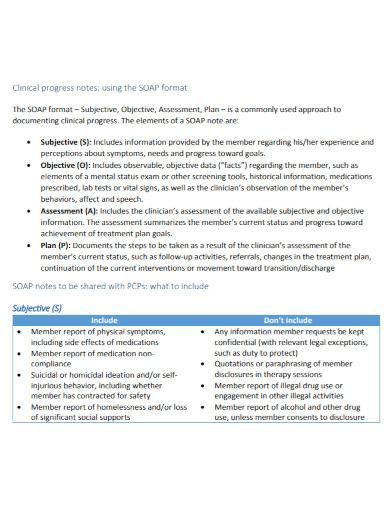
2. Clinical Soap Note Assessment
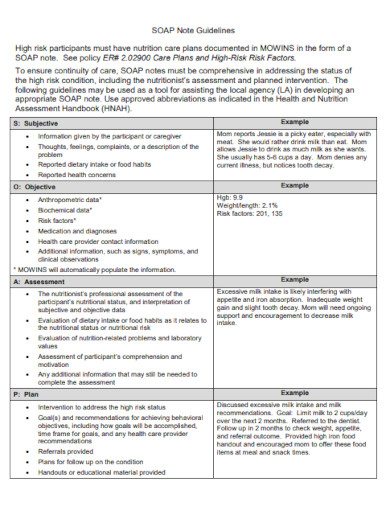
3. Soap Note Nutritionist Assessment
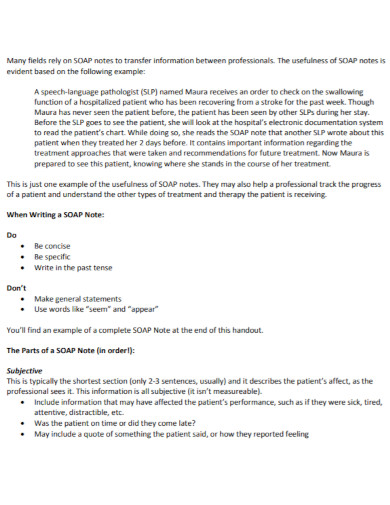
4. University Soap Note Assessment
Definition of SOAP
Have you ever encountered this word SOAP? Did you know that this is merely an abbreviation and the full meaning of the word is different? SOAP actually means Subjective, Objective, Assessment, Plan/Procedure. Now that we know what this abbreviated word means, let’s move on to the general definition of the term. Subjective, Objective, Assessment and Plan is an acronym referring to a method used mostly by healthcare professionals. This document is used by healthcare as it is more structured and in an organized way. Imagine a table where you are going to put the correct information, that is how SOAP Assessment helps them.
Definition of Assessment
An assessment is a type of examination that allows the assessor to check, analyze, and evaluate a person or an object. The act of assessing something or someone to see if they are still up to the task of handling things. The process of gathering data, interpreting the results and evaluating to check if there is any improvement whatsoever. A systematic basis of examination where the assessor processes the results and information they have gathered for educational purposes.
Definition of SOAP Assessment
A SOAP note assessment is a method on which healthcare professionals and providers use to take down notes of a person’s charts. In addition to that, it also gives out other information provided that it follows the SOAP method. This type of assessment helps healthcare providers and professionals to easily take down information without having to write the whole thing. As well as having to write the full information without missing some bits or pieces of it. Lastly, this type of method is mostly used by people in the medical field as they are more likely to assess the patient’s outcome and plan what to do next.
Importance of SOAP note assessment
The importance of this method for assessing is that relevant data are easier to find. As well as everything you may need is immediately there. The reason for this method is to make sure that all the data that has been collected are easily given for use. The advantage of using this method is to organize all the information in one location for easier search. Take it like a file folder with all the detailed information. It would be easier to store them in one folder than to store them in different places. It lessens the time for looking and more into finding.
Tools Used for SOAP note assessment
Check out the tools you may use when writing your SOAP note assessment, Each tool differs in forms but are generally used for assessment purposes:
- Bullet form
- Narrative form
- Outline
- Table form
- Diagram
Tips for Writing SOAP note assessment
Here are some tips to help you get started on writing your SOAP assessment. Remember these tips are merely suggestions. How you write your assessment and how you construct it using the tools above, is merely up to you.
- Follow the SOAP format
- Keep confidential information out of the assessment
- Your objective has to be specific and realistic
- Assess and give realistic examples
- Take note of your grammar and spelling
- Keep notes on your assessment for future purposes
FAQs
How important is this method of assessment?
Very important. Especially if you are one working in the medical profession and healthcare profession. As notes are important, as well as the information given, it is best to use the SOAP method to make your notes clearer and less confusing.
What should be avoided when writing the Objective part of the note assessment?
Avoid writing not so realistic objectives. As your objectives are also a part of the assessment and looking for the answer to the problem.
Who is the audience for this SOAP assessment?
The people who may be reading your SOAP note assessments are your colleagues, yourself and your superiors. You must always remember to follow the format. Keep in mind that this format is used to make note writing easier as well as easier to find for medical purposes.
Is there another thing I should watch out for in this method of assessment?
Apart from remembering the format of your notes, you must also remember to take down important information. Which would become useful in different situations. Keep your notes clear and concise all the time.
Anyone working in the healthcare industry knows very well that keeping your notes intact, clear and concise can be a challenge. Especially when information plays an important role in this. Rather than having to keep up with writing about a patient’s history, using the SOAP method can help lessen the problem.