10+ Therapy Progress Note Examples to Download
All types of progress notes should be made concisely and accurately. Therapy requires to be flexible at all times so you have to use various techniques in helping out your clients. Therapists, on the other hand, are responsible of using an effective approach to see if something is working well or not. In doing so, they make use of therapy progress notes to monitor a patient’s progress. As you go along with this article, you will be able to know what a therapy progress note is all about and how to effectively create one.
10+ Therapy Progress Note Examples
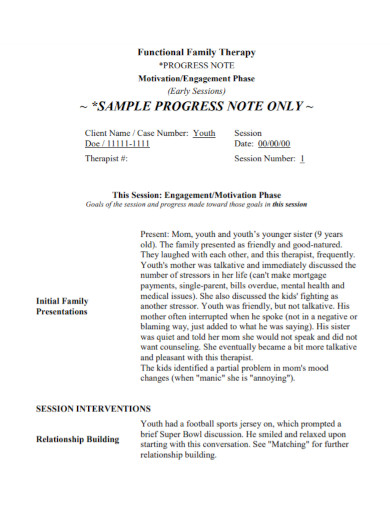
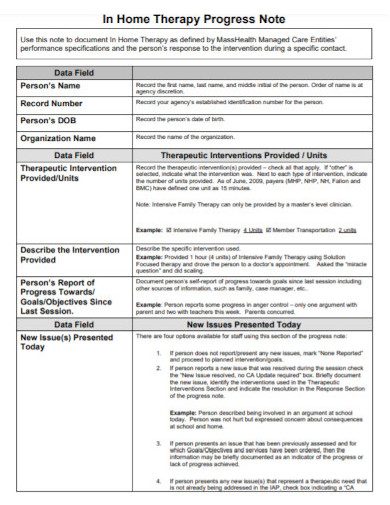
1. Family Therapy Progress Note
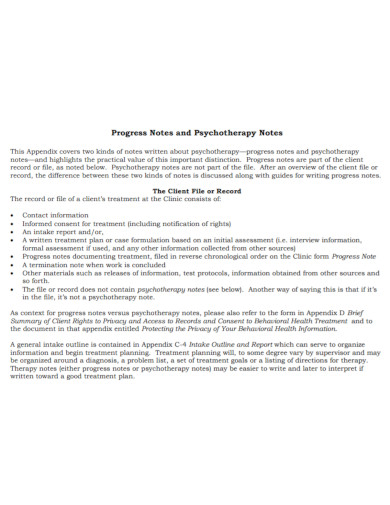
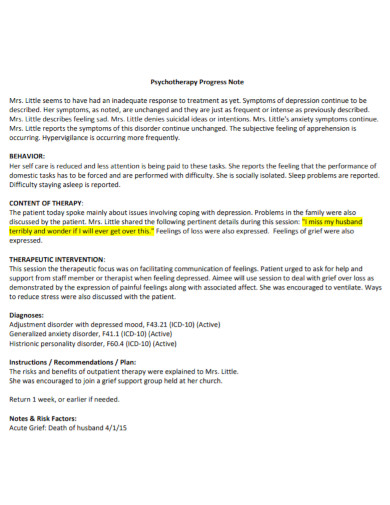
2. Psychotherapy Progress Note
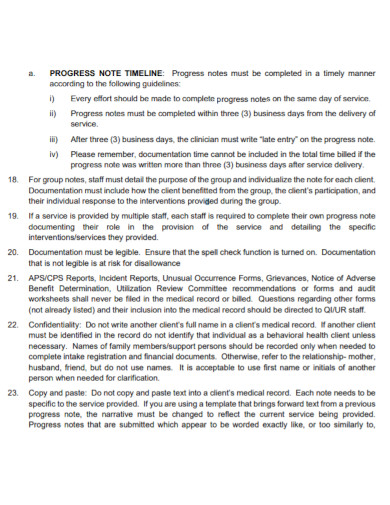
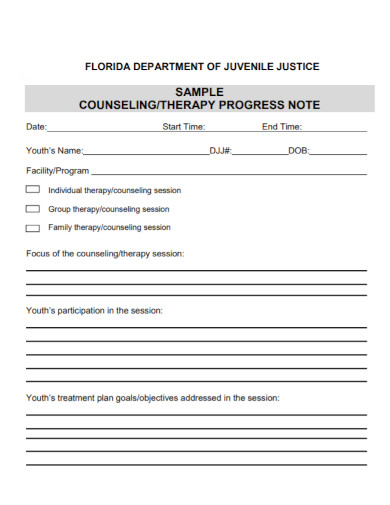
3. Clinical Therapy Progress Note
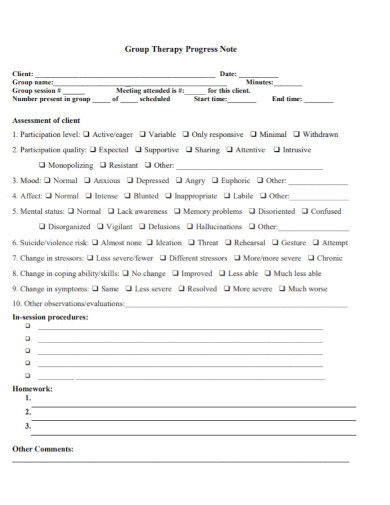
4. Group Therapy Progress Note
5. Home Therapy Progress Note
6. Depression Anxiety Therapy Progress Note
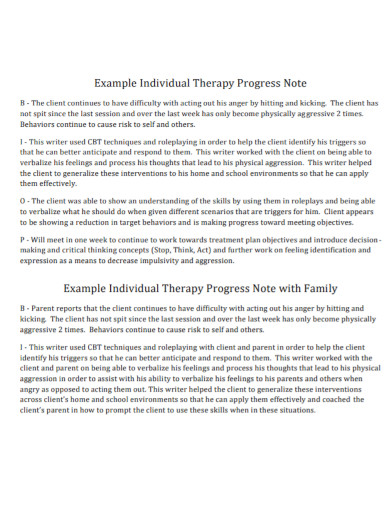
7. Individual Therapy Progress Note
8. Therapy Progress Note Documentation
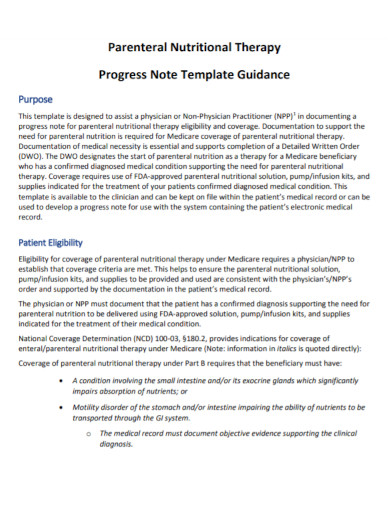
9. Nutritional Therapy Progress Note
10. Standard Therapy Progress Note
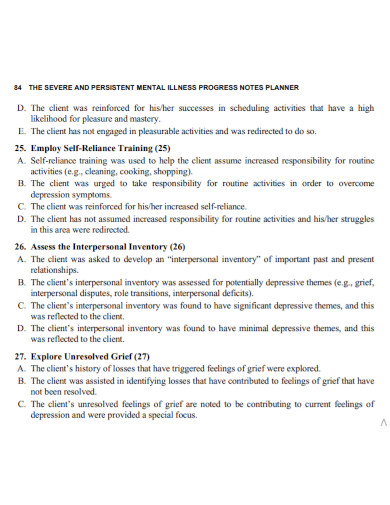
11. Mental Illness Therapy Progress Note
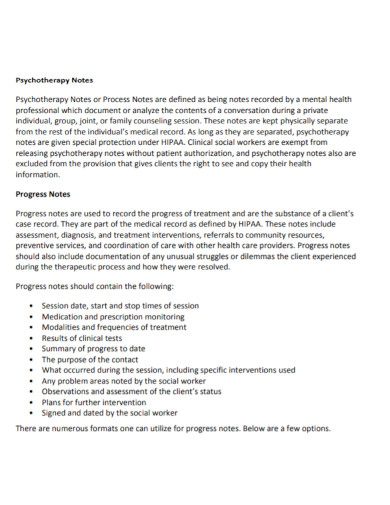
What is a Therapy Progress Note?
A therapy progress notes are clinical notes that involve the details of the patient’s treatment and care. They contain facts and the process about the type of care a patient receives as well as the diagnosis and treatments. They are considered to be documents that provides communication about a patient’s information with regards to his or her condition.
Templates for Progress Notes
Therapy progress notes do not follow a specific format. However, there are templates that you can use for your progress notes.
SOAP Template
The SOAP note or template is comprehensive and can be used when summarizing. SOAP stands for Subjective, Objective, Assessment and Plan. Subjective section is about the perspective of the clients. It includes some information about the patient, the effectiveness of the therapy, progress of the session and more. Objective section shows your observation about the client’s attitude, their response to interventions and the results. Assessment section includes evaluation data and the records of your opinion. Plan section includes your action such as the way on how you are going to address the next session and how can you relate those plans to the client’s treatment goals.
DAP Template
This template is considered as user-friendly which eventually stands for Data, Assessment, and Plan. The data refers to the information you have gathered during the sessions including your own observations. The assessment refers to the act of synthesizing the data you have gathered. It interprets the progress of your client. The plan refers to how are you going to take action in order to achieve the desired treatment plan and goal.
BIRP Template
This template makes an easy understanding about a client’s response with regards to his or her interventions during the session. BIRP stands for Behavior, Interventions, Response, and Plan. Behavior is where the client and the therapist finds their home using each of the subjective and objective data. Intervention is where you are going to keep the records that are useful in achieving a goal. Response is your client’s reaction. Plan is when you are able to finalize the focus and schedule of your next session.
Steps in Writing Effective Progress Notes
- Put an overview of the session information including the name of the practitioner and the patient, the place, duration of session and the type of service.
- Write the diagnosis.
- Put a description of how the patient appears to be.
- Provide an information about the patient’s well-being.
- Include in the progress notes the medications that the patient is using.
- Include the report about the status of the patient whether he or she is feeling something or has any progress after a few session.
- Put the results of the tests, documents, etc.
- Determine the type of intervention used.
- Mention the client’s treatment plan.
- Sign the documents for validity.
FAQs
What are the frequently used interventions?
Anger management, coping strategies development, identifying triggers, mindfulness, imagery, stress management and more.
What intervention should be used when dealing with trauma?
In dealing with trauma, they use the eye movement desensitization and reprocessing intervention during the counseling session.
What is the difference between having a group progress notes and individual progress notes?
Group progress notes do not identify information for the clients while the individual progress notes describes how an individual client engage within the group including the information about the diagnoses, treatment plan, etc.
Those treatment plans and progress notes help you in understanding your clients better. Progress notes serves as your guide to deal more about the patient treatment plan to meet their needs. This may be done by group or individually, but always be aware of the scope each category has.


![10+ Therapy Progress Note Examples [ Clinical, Anxiety, Illness ]](https://images.examples.com/wp-content/uploads/2021/05/10-Therapy-Progress-Note-Examples-Clinical-Anxiety-Illness-.jpg)