19+ SOAP Note Examples to Download
Health care providers, such as doctors, clinicians, physicians, and nurses as well as medical interns use a SOAP note to communicate effectively to their colleagues about the condition of the patient as it is essential when providing a cure for the diagnosis and giving medical or surgical treatment. SOAP note facilitates a standard method in showing patient information.
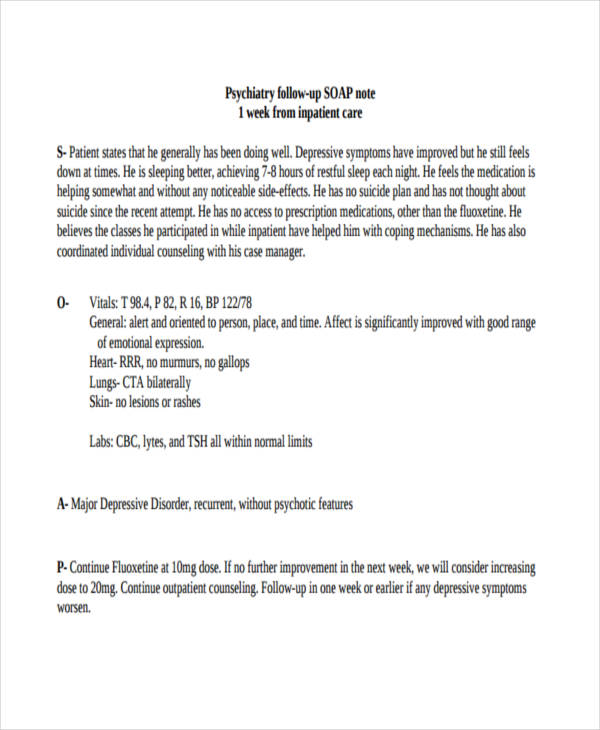
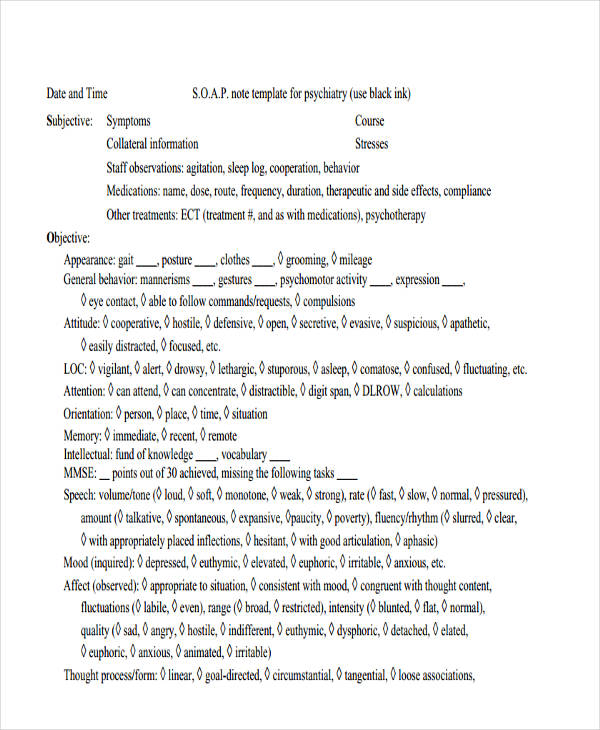
Psychiatric SOAP Notes
Psychiatry Follow-Up SOAP
Psychiatric SOAP Example
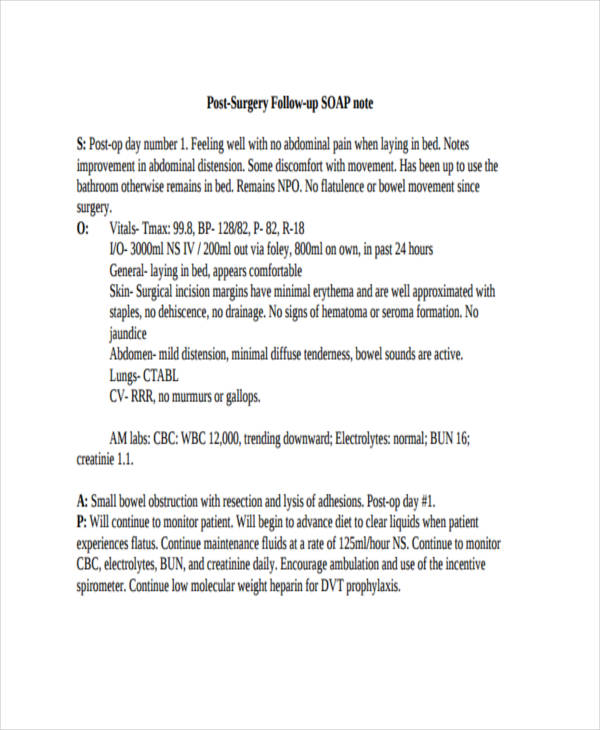
Surgery SOAP Note
Post surgery Follow-Up Note
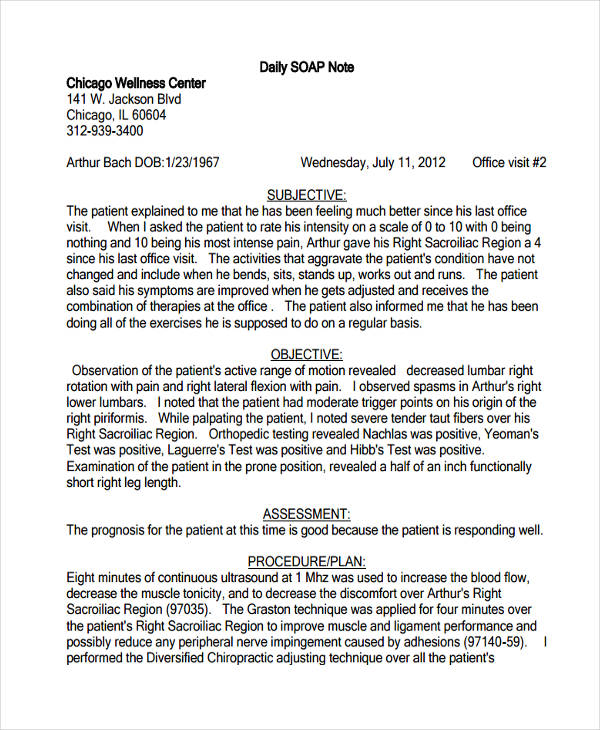
Daily SOAP Note
Daily SOAP Sample
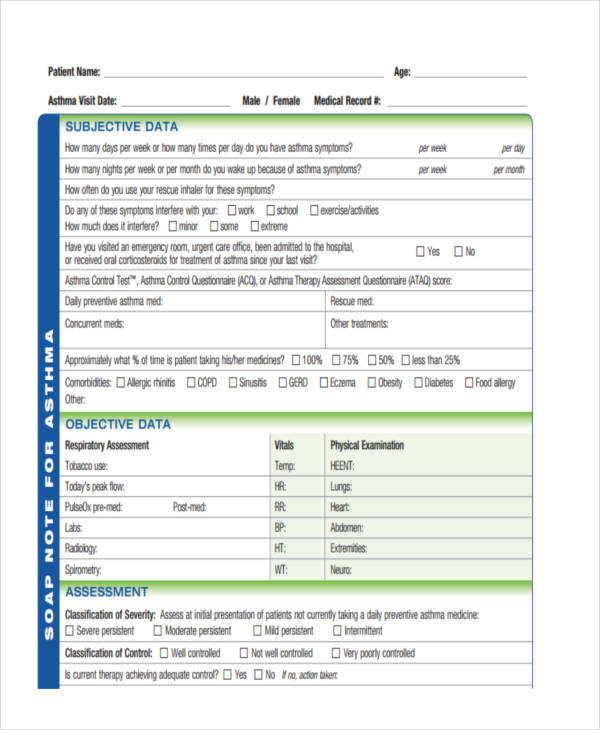
Asthma SOAP Note Example
Asthma SOAP Note
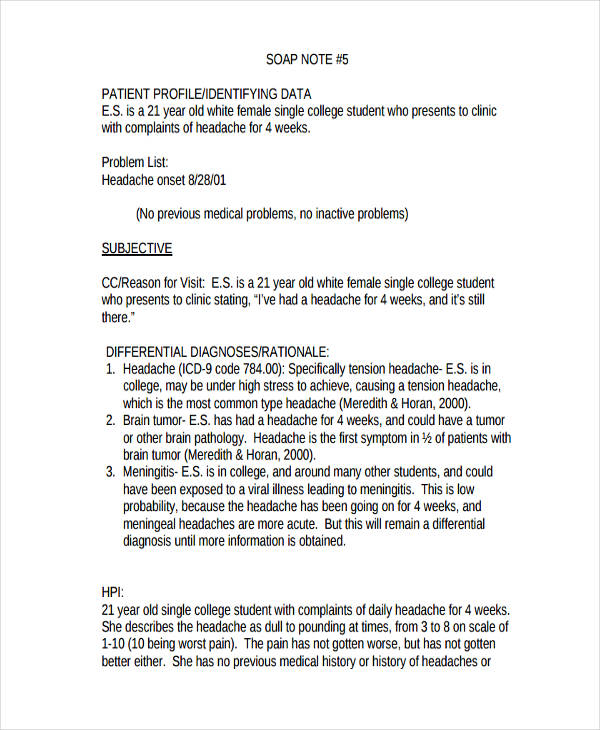
SOAP Note Example
Patient SOAP Sample
Prenatal SOAP
SOAP Note Sample
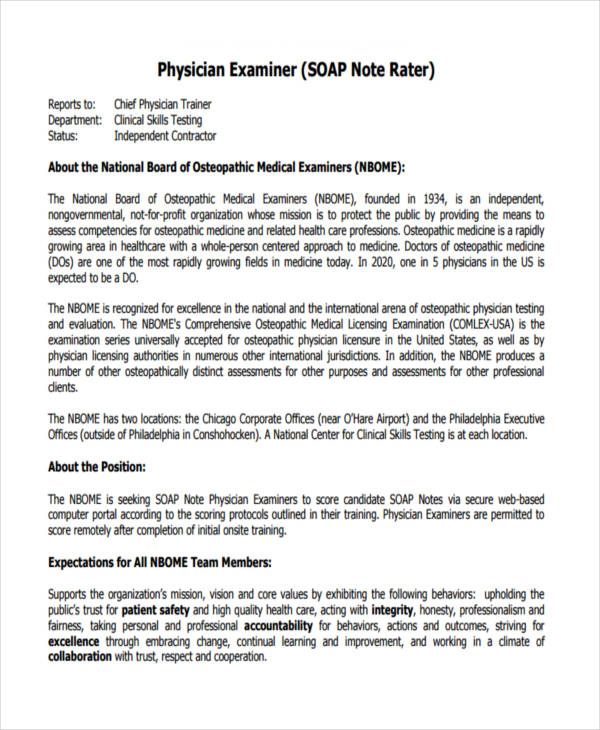
Physician SOAP Note
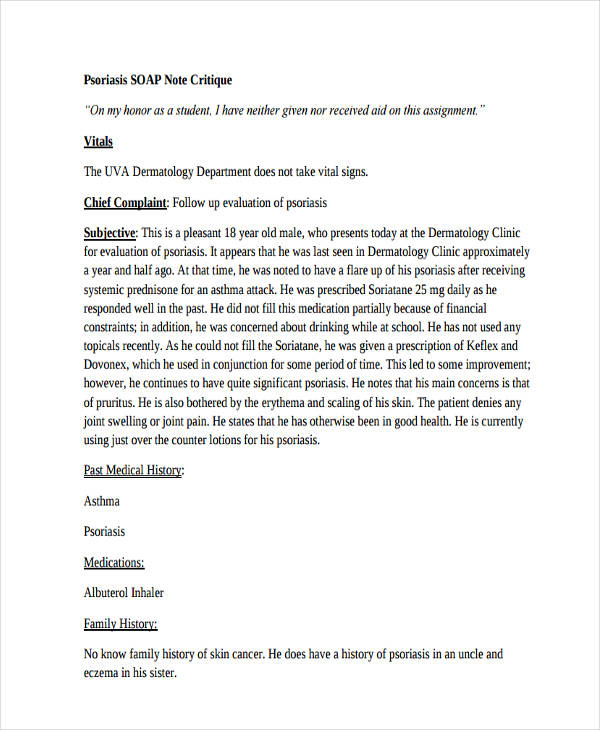
Psoriasis SOAP Sample
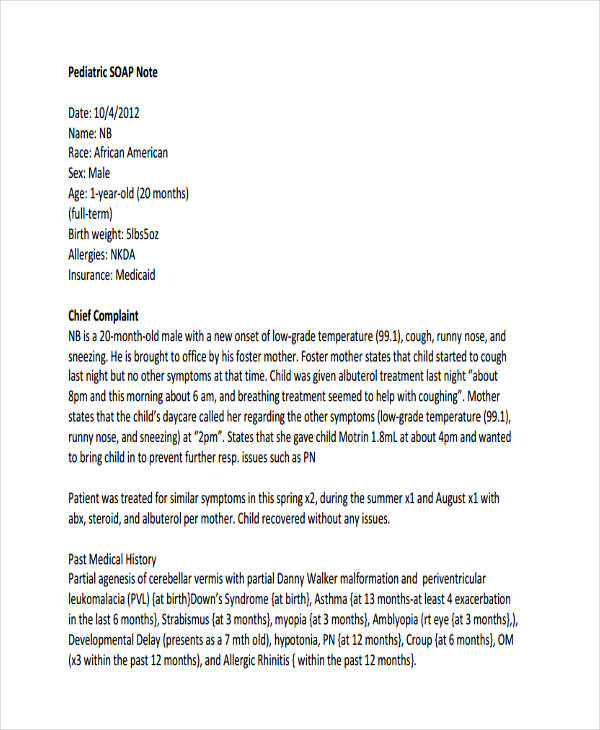
Pediatric SOAP Example
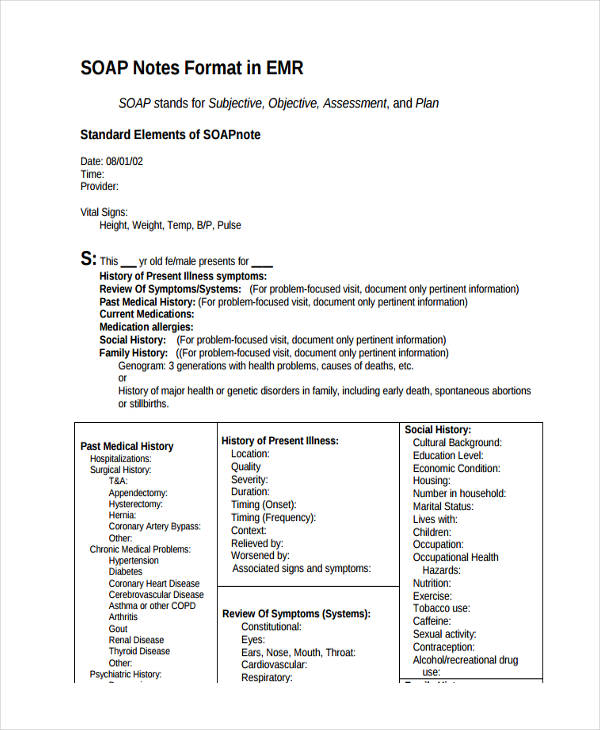
SOAP Note Format
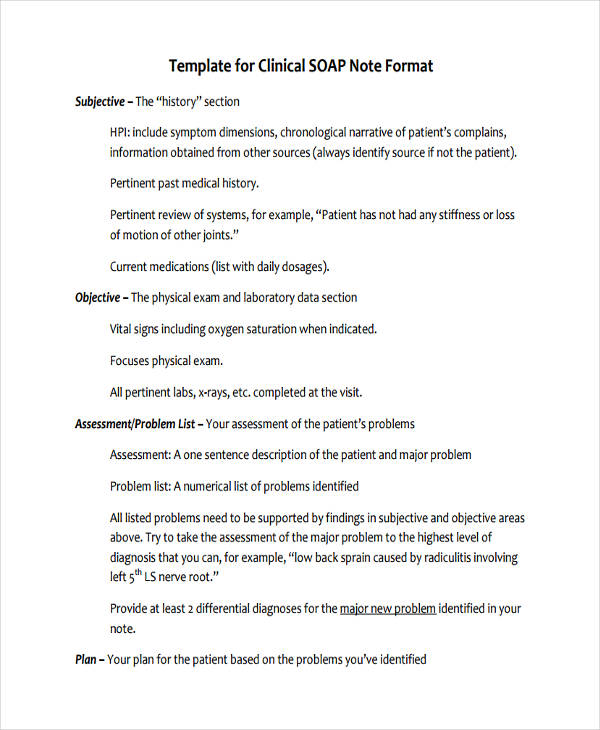
Clinical SOAP Note
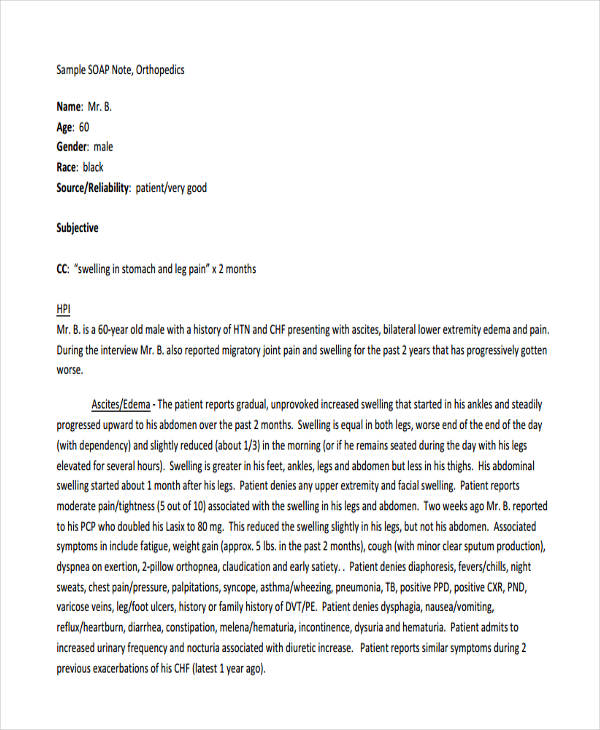
Orthopedic SOAP Example
SOAP Note Example
SOAP Note in PDF
Sample SOAP Note
Simple SOAP Note
Basic SOAP Note
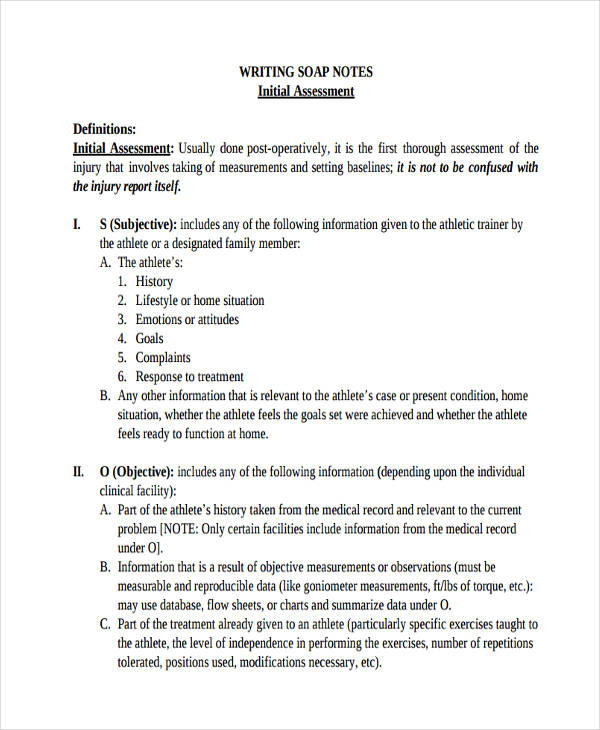
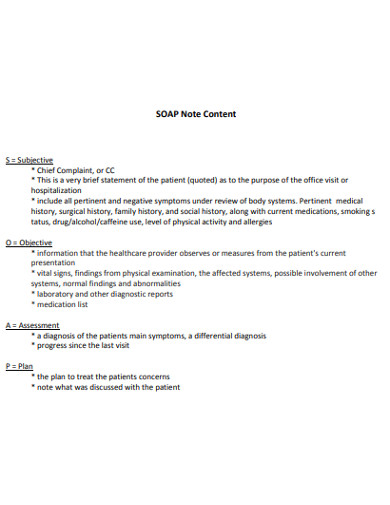
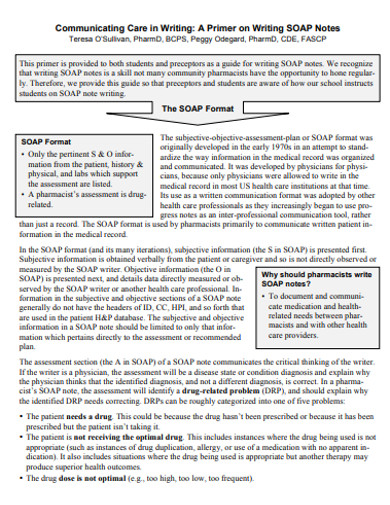
What Is a Soap Note?
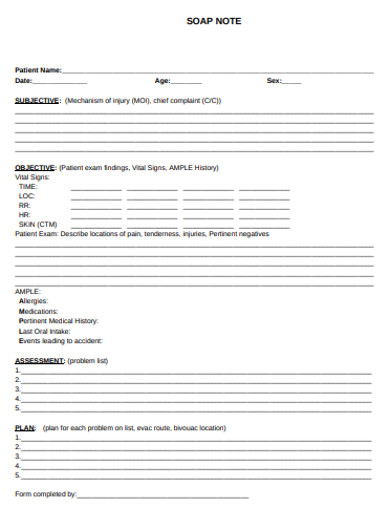
A printable SOAP note is a method of documentation that is employed by health care professionals to write data and records to make a patient’s char, along with other documents. Check progress notes for more. Health care providers including doctors and clinician use a SOAP note to have a standard format for organizing patient information as well as the patient’s medical conditions and issues.
How to Write a Good Soap Note
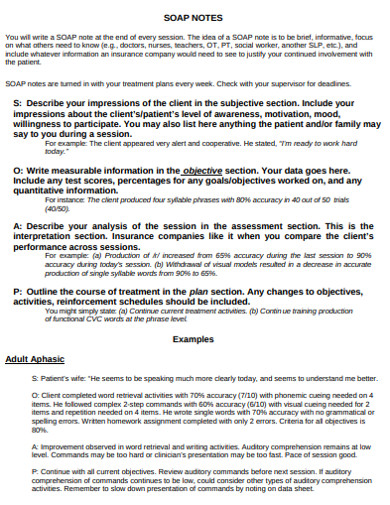
An effective soap note helps when you are going to be taking down every note about the patient and the progress of the patient. An effective soap note also helps when you are going to go through the general to specific details you wrote. How to write a Soap note? To write an effective SOAP note, you must follow the format that is mentioned below:
Step 1: Write a Thorough Soap Thank-You Note
Write a thorough SOAP thank you note that you can refer to during rounds. It is hard to remember specific things about an individual patient, such as lab results, vita sins, etc. Organize your thoughts before writing a SOAP note. Ask yourself if do you have to write everything in the same orders as the patient expressed it.
Step 2: Take Your Time in Writing
Take your time in writing the information that you need to include in your free note. Do not overload your note with too many details. If you have only the total information, then make the formal report because adding some basic information will not help. If the patient doesn’t feel a specific pain, then you do not have to write it.
Step 3: You Are Writing for Other Health Care Providers
It is acceptable if y9ou use medical terms and abbreviations to make the SOAP notes brief. You must also know what short forms are acceptable and easily understandable. You can also take a look at the therapy note samples that are available online for more.
Step 4: Note Should Only Last for Five Minutes When Presenting
Your note should only last for five minutes when presenting it. If your blank notes are organized and well-structured then you can present it at least five minutes. You can also use the standard SOAP formats, which can help you organize your notes in the most effective way possible.
FAQs
What are the four parts of a Soap note?
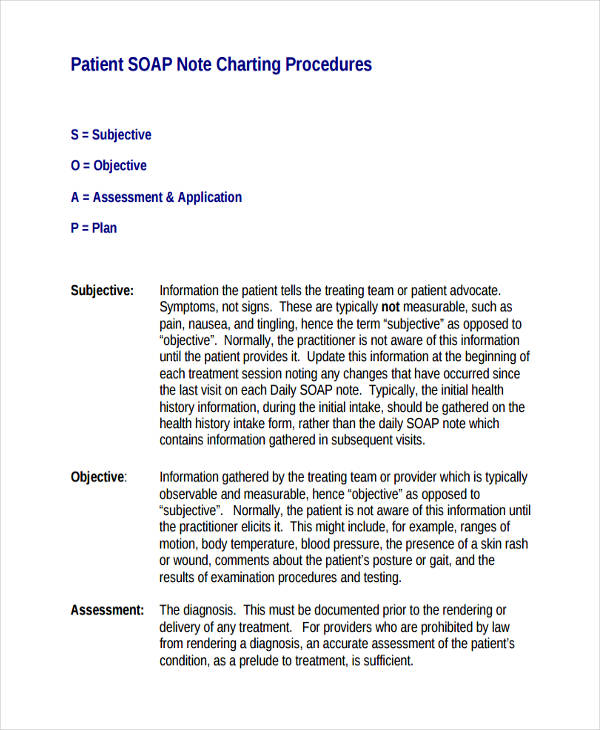
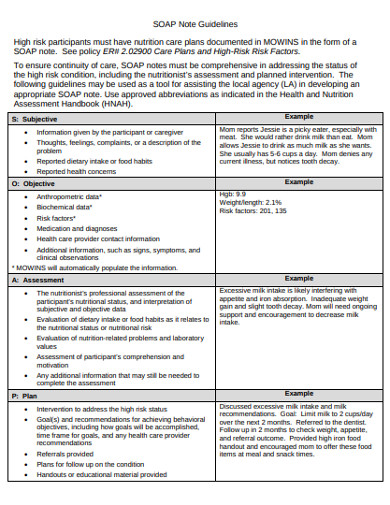
The four parts of a Soap note are subjective, objective, assessment, and plan. Write your impressions on the patient. This also includes the patient’s levels of awareness, mood, willingness to participate, etc. Followed by the objective portion. Write all the measurable data, such as vital signs, pulse respiration, and body temperature. Then the assessment portion or the interpretation of the diagnosis, and lastly the plan. How you are going to address the patient’s issues. Check nursing note samples for more.
What does the subjective part include?
This is the generic subjective parts to expect in a Soap note. We have: onset, location, character, alleviating factors, radiation, and additional symptoms.
What is the difference between subjective and objective in a Soap note?
The subjective part describes the patient’s condition in the form of a narration. This is where you make your observations based on the condition or complaint which the patient expresses verbally. This also shows why the patient came to the doctor in the first place for the doctor’s note. This part of the note contains measurable data as this involves data that you can hear, smell, see and feel. So, dealing with your sensory organs. This also includes the patient’s condition or data that are repeatable and traceable.
A SOAP note has its benefits that provide systematic documentation and evaluation to every individual patient’s condition. Nonetheless, on the other hand, there are shortcomings concerning its usage. Overall, this kind of SOAP notes is pretty effective and useful. though there is always room for improvement.