9+ Hospital Discharge Letter Examples to Download
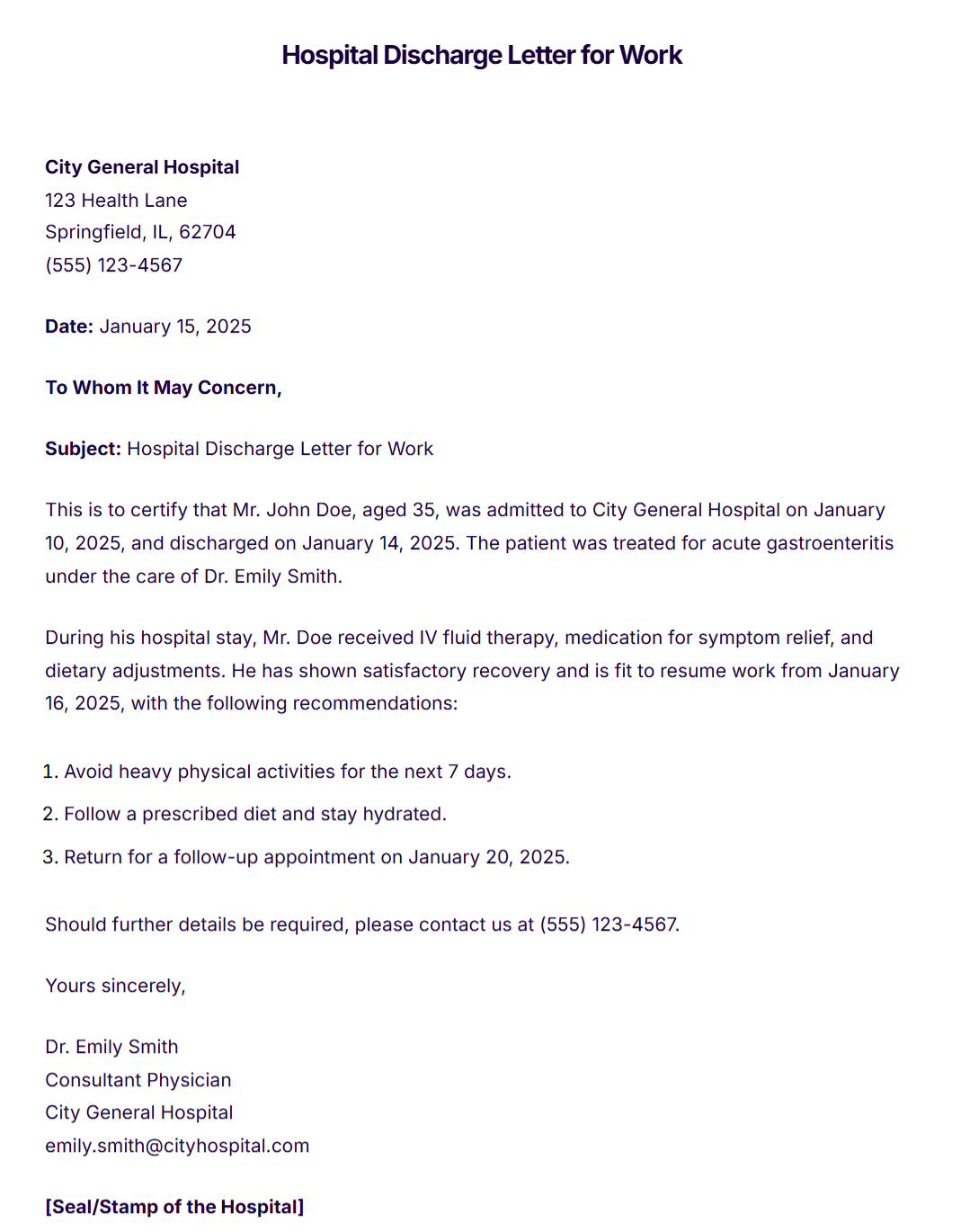
After a patient stayed in the hospital to get proper treatment, they will receive a letter or document from the physician indicating that they will be discharged. It is essential because it informs the immediate family and the patient itself about his or her condition before, during and after being an inpatient. This is similar to a discharge summary report. In this article, you will be able to know about what a discharge letter is and how to create one.
What is a Discharge Letter?
A discharge letter is a short summary of the details of the patient’s hospital admission together with the medications and other treatment he or she has received. It is usually prepared or written by the patient’s attending physician.
Once a patient is declared healthy, the attending physician can already write a discharge letter so that the patient may continue his or her rest at home. Hospital discharge letters will indicate all the details starting from the time of admission to the time that the patient has been released, all the diagnoses and the procedures, medications, follow-up instructions and recommendations.
Content of a Discharge Letter
The letter starts with the demographics.
- Patient’s name
- Date of birth
- Identification number or Patient’s number
- Sex
- Emergency contact (this includes the full name and the relationship of the person to the patient and contact number)
It can be followed by the hospital details.
- The name of the discharging consultant of the patient
- The name of the department that is responsible of the patient
- Date and time of both the admission and discharge
- Destination of the patient after being discharged (home, another hospital, etc.)
Next is the complete details of the plan on how to manage a patient after discharge.
- List of treatments and medication or surgery
- Follow-up treatments
- Referrals made by the hospital
After that is the summary of the changes in patient’s medication with its corresponding explanation as to why there have been changes. Next on the list is the medications that a patient needs to take home. For each medication, you have to put the generic drug name or specific brand name, the form of the medicine (capsule, syrup, tablet, etc.), the number of times it should be taken in a day, the indication and some additional instructions.
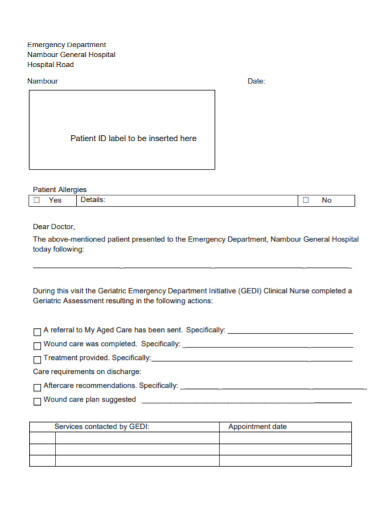
It is also important to indicate allergies and adverse reactions that a patient may experience after taking medications. The physician may indicate what caused the allergic reaction, the manifestation or the type of reaction shown and when was the allergic reaction occurred.
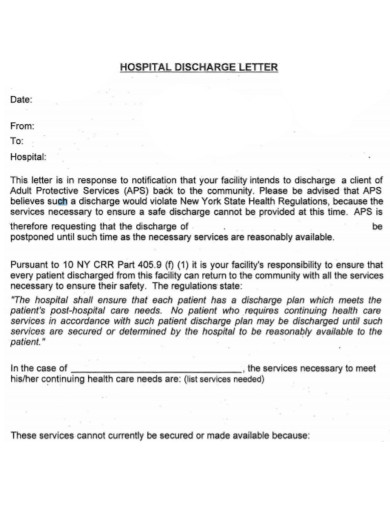
Discharge letters includes summary information about the patient’s hospital stay. Just like this example;
“You were admitted to South General Hospital due to skin swelling, stomach ache and difficulty in breathing. We had a lot of tests to see about the issue. You should continue taking ________________ to help stop pain of the swollen area… Should you have any concerns, contact your attending physician.” (Geeky Medics, 2020)
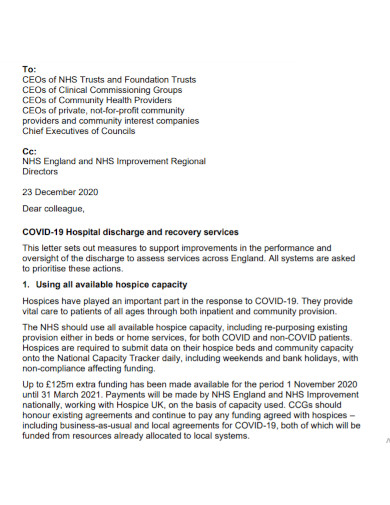
Hospital Discharge Letter for Work
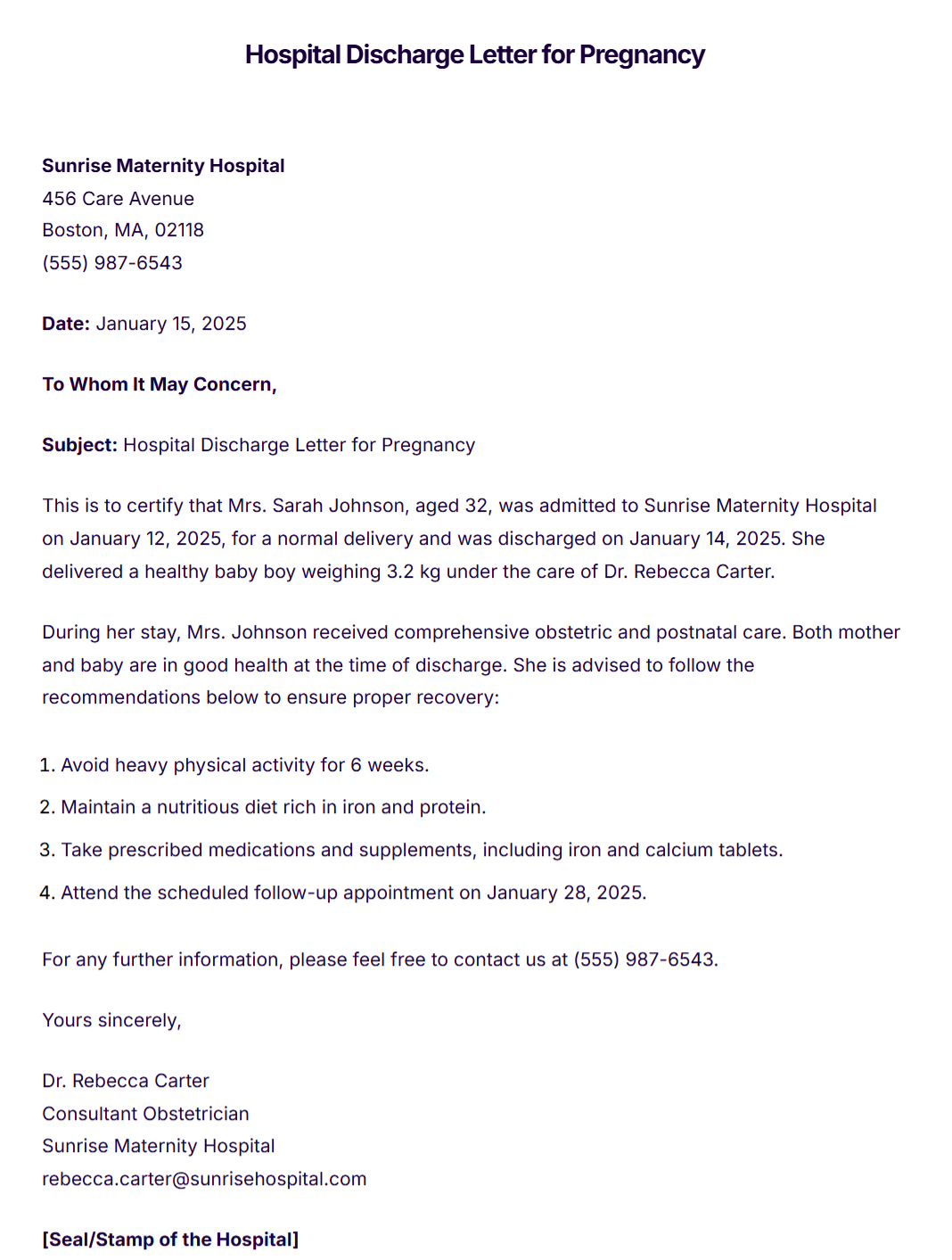
Hospital Discharge Letter for Pregnancy
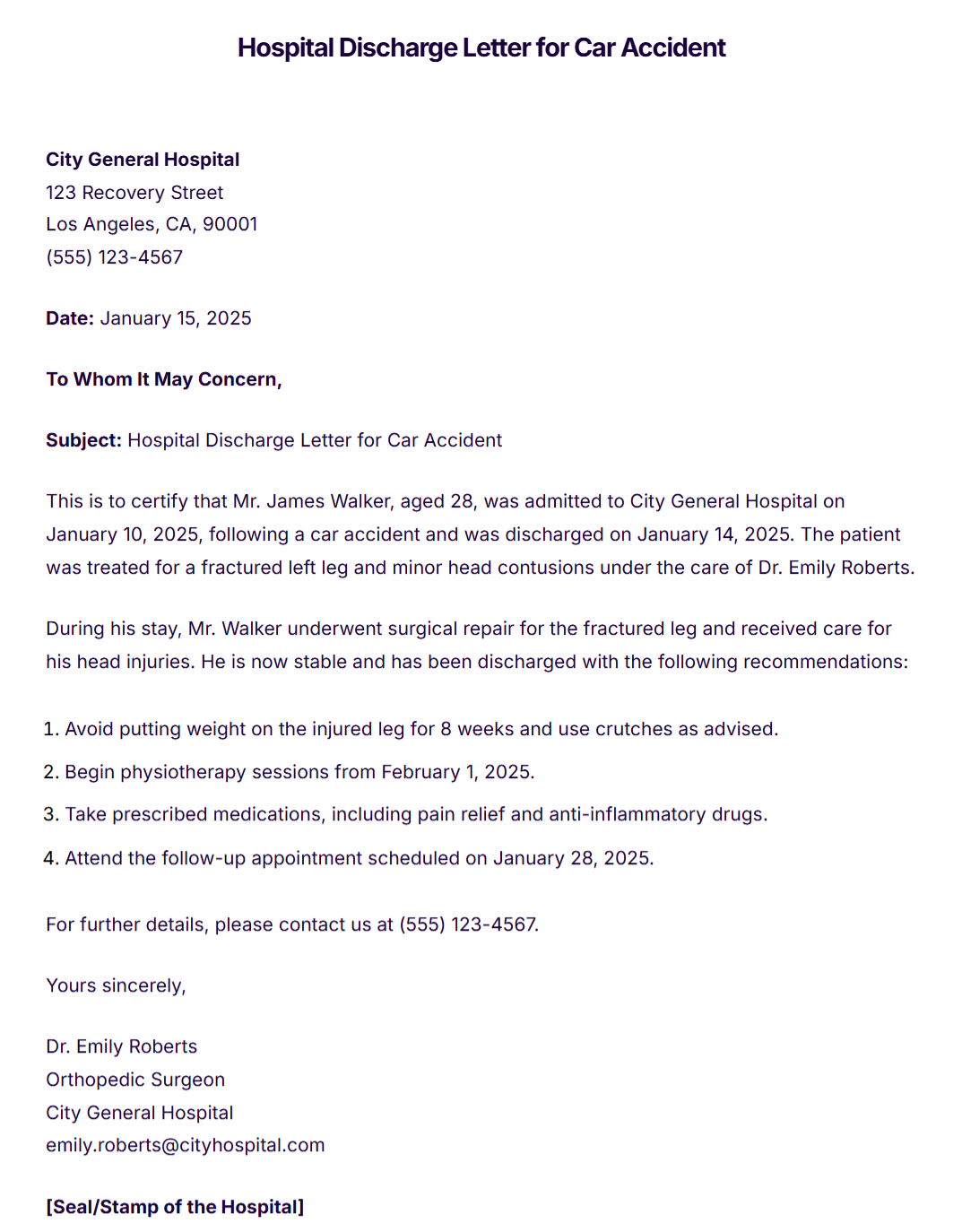
Hospital Discharge Letter for Car Accident
Inpatient Hospital Discharge Letter

Hospital Discharge Letter Template
Hospital Nurse Discharge Letter
Medical Hospital Discharge Letter
COVID-19 Hospital Discharge Letter
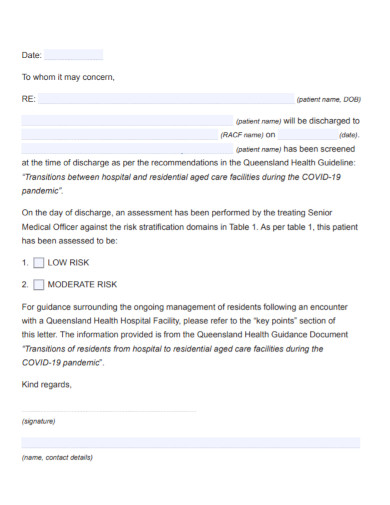
Residential Hospital Discharge Letter
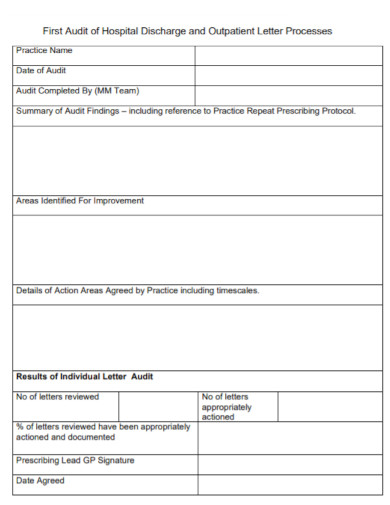
Hospital Discharge Outpatient Letter
How to Write a Hospital Discharge Letter
1. Start with Hospital Information
- Include the hospital’s name, address, contact number, and logo at the top.
2. Date and Recipient
- Mention the date of issue and write “To Whom It May Concern” or the intended recipient (e.g., patient, employer).
3. Subject Line
- Add a clear subject like “Hospital Discharge Letter for [Patient’s Name].”
4. Patient Details
- State the patient’s full name, age, and admission and discharge dates.
5. Diagnosis and Treatment
- Provide a brief summary of the condition or diagnosis for which the patient was treated.
- Mention the treatments, procedures, or tests conducted during the stay.
6. Condition at Discharge
- Indicate the patient’s health status at discharge (e.g., stable, improved).
- Include whether they are fit for work or need further rest.
7. Medications and Instructions
- List prescribed medications with dosages and durations.
- Provide specific care instructions (e.g., dietary restrictions, physical activity limits).
8. Follow-up Recommendations
- Mention the follow-up appointment date and any additional tests required.
- Provide emergency contact details for immediate concerns.
9. Doctor’s Details and Signature
- Include the treating doctor’s name, designation, and contact information.
- Add the doctor’s signature and the hospital’s stamp or seal for authenticity.
10. Optional Annexures
- Attach supporting documents like test results, prescriptions, or referral notes if necessary.
Tips for Writing Hospital Discharge Letter
- Keep it concise: Avoid unnecessary medical jargon; use simple language.
- Be specific: Mention all relevant details about treatment and post-discharge care.
- Maintain professionalism: Ensure the tone is formal and the document is error-free.
- Ensure legibility: If handwritten, ensure neatness; otherwise, use a typed format.
FAQs
Can a patient get his or her own copy of a discharge letter?
Yes. Each patient must receive a copy once they got home. If you have not received any, ask your physician or nurse to get one.
Is there such thing as discharge planning? If yes, how is it done?
Discharge planning is done after a patient has been admitted to a hospital or a few days before the physician’s estimated date of discharge.
What happens if a patient leave the hospital before the date of discharge?
Leaving the hospital before your date of discharge can be risky. It is either the patient will have the chance for rehospitalization or the patient will not be able to receive proper treatment making him or her get a severe condition of his or her illness.
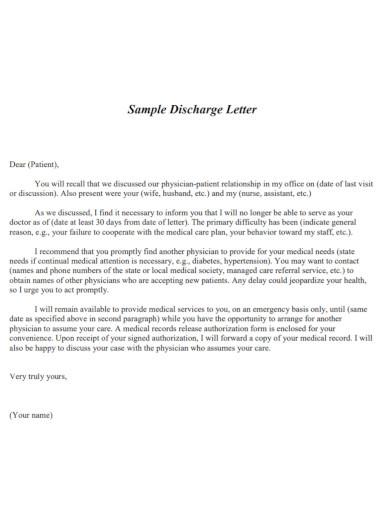
Discharge letters and any other documents are necessary for both the patient and the physician. It will serve as a medium of communication that tells about the details of the patient’s condition. At the end of ever discharge letters show the signature of the physician and the date when the letter has been signed.