10+ Discharge Summary Report Examples to Download
Hospitals require their medical personnel to submit their discharge reports or summary. It is considered as one way of communicating to the primary care physician. Not only that but it also ensures the safety of the patient. In the medical field, all the documents must be factual and accurate. This is applicable to any records including a discharge summary. In this article, you will be able to know what a discharge summary means and how to create one.
10+ Discharge Summary Report Examples
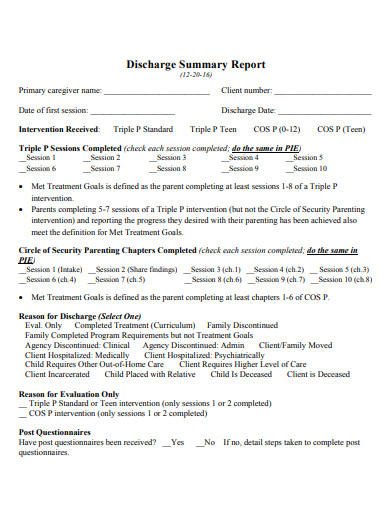
1. Parenting Discharge Summary Report
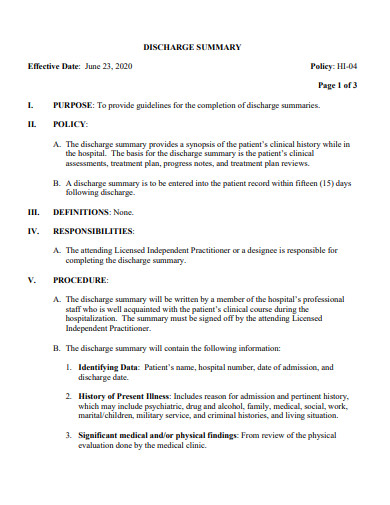
2. Hospital Discharge Summary Report
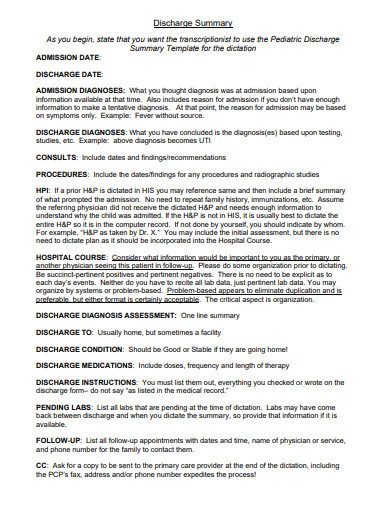
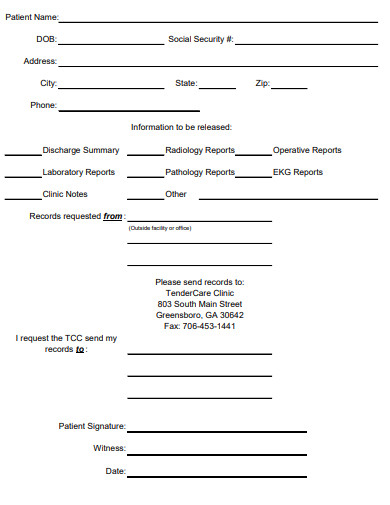
3. Printable Discharge Summary Report
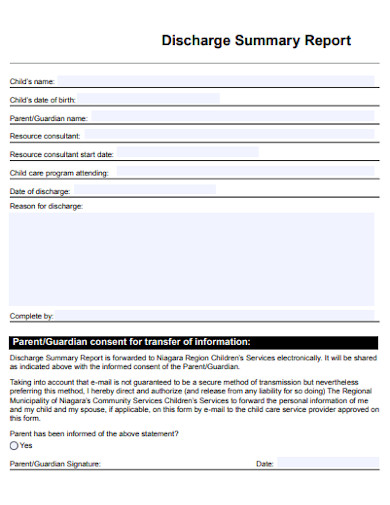
4. Editable Discharge Summary Report
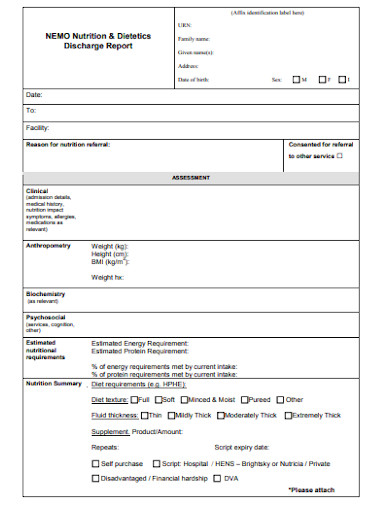
6. Nutrition & Dietetics Discharge Summary Report
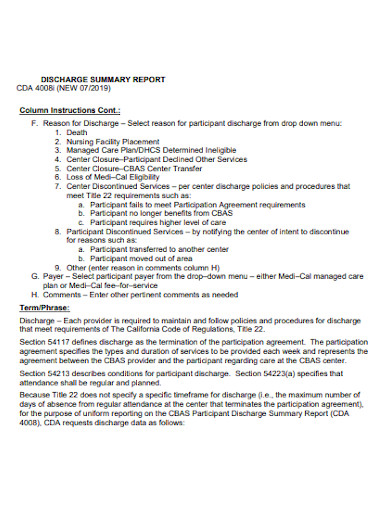
7. Simple Discharge Summary Report
8. Professional Discharge Summary Report
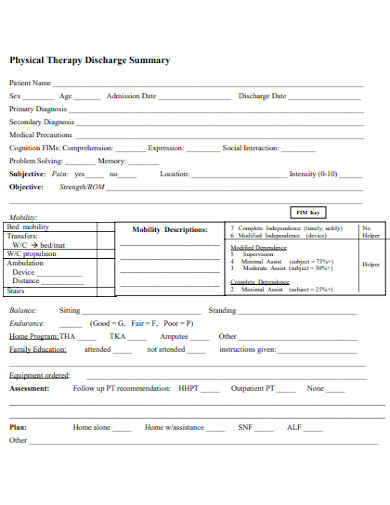
9. Physical Therapy Discharge Summary Report
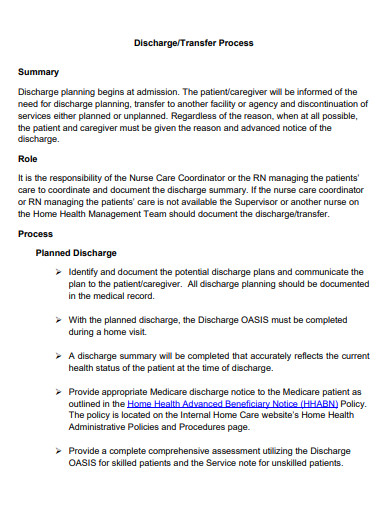
10. Discharge Transfer Summary Report
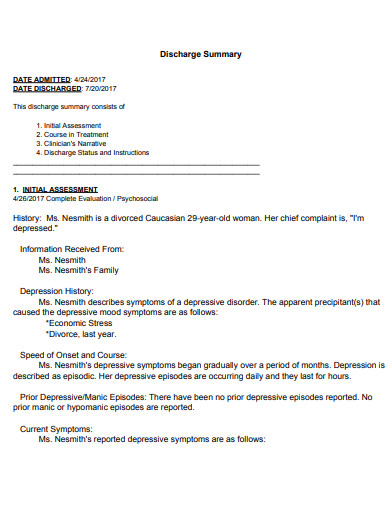
11. Discharge Initial Summary Report
What is a Discharge Summary?
A discharge summary is a type of letter written by physicians to record the reason why you got admitted, the results of the tests, the list of your medication and the follow-ups that you needed. This is considered essential especially when you are going to transfer information to the primary physician assigned to a particular patient. This should contain relevant information pertaining to the patient’s condition.
Importance of Discharge Summary
The physician and other medical personnel assigned to a particular patient has the right to know about the patient’s condition during his or her stay at the hospital. Providing a discharge summary would help the implementation of the correct coordination of care and transition of the patient.
- It helps improve the discharge process – individuals assigned in the transition of a patient would always look for ways to improve the discharge process. this includes the discharge planning, enlisting of medications and follow-up appointments.
- It serves as the mode of communication between the hospital care team and aftercare.
Content of a Discharge Summary
- It should indicate the reason of hospitalization indicating the patient’s diagnosis
This includes the description of the patient’s condition and initial presentation of his or her condition during admission.
- Indicate the significant findings
This refers to the primary diagnoses.
- Indicate the procedures performed such as the treatment and services provided to the patient
This includes the description of what occurred to a patient during his or her stay in the hospital or a description of a certain treatment that a patient experienced as inpatient.
- Indicate the condition of the patient at discharged
This refers to how the patient is doing nd his or her overall status during discharge.
- Indicate the education provided to the family and also to the patient
This refers to the discharge medications, therapy orders, dietary instructions, instructions for follow-up check ups and the like.
- Indicate the list of medication given to the patient
- Indicate the list of the tests that were still unavailable during the time of discharge
At the end of every discharge summary is the signature of the attending physician. It could be electronic or physical.
The six (6) components stated already serves a great foundation but it would be more accurate to add more on the list to improve patient safety. This includes:
– Person’s name and contact number in case of emergency
– Possible interventions, wound care, etc.
FAQs
Is there a process to follow in doing a patient discharge?
When you leave the hospital after a treatment, you will be issued a patient discharge summary. This is to be written and signed by the attending physician together with the necessary details of the patient during his or her stay.
When can a patient be discharged?
A hospital will be able to discharge a patient when he or she no longer needs inpatient treatments. They can also discharge you if they are to transfer you to another facility.
Is the patient accompanied by a health worker during a discharge?
The patient will be accompanied by a medical personnel because it is part of the hospital’s protocol. Some medical personnel would still assess your condition despite being discharged.
Discharge summary reports play a vital role in informing the immediate family about the patient’s condition during the duration of his or her stay in the hospital. It has to provide true details about the patient in observance of the hospital’s protocols. Following the right contents would make it concise and accurate.